11 September 2020: Articles 
Role of Long-Term Vestibular Rehabilitation in a Patient with Posterior Fossa Tumor: A Case Report with 2 Years of Follow-Up
Unusual clinical course, Challenging differential diagnosis
Yuşa Başoğlu1ABCDEFG*, Oğuz Yilmaz1ABDG, İlayda Çelik1BEF, Mustafa Bülent Şerbetçioğlu1BEGDOI: 10.12659/AJCR.924262
Am J Case Rep 2020; 21:e924262
Abstract
BACKGROUND: Lhermitte-Duclos disease (LDD) is caused by a rare slow-growing mass in the cerebellum. LDD generally is experienced by young adults, but also it has been encountered in the pediatric population. Lhermitte and Duclos first described cerebellar dysplastic gangliocytoma in 1920. The first case they described included occipital headache, paroxysmal vertigo, falls, hearing problems, and memory deficits. Our patient had typical symptoms of the disorder such as headache, nausea, vomiting, blurred vision, and imbalance. The purpose of this case report was to describe the outcome of a computerized dynamic posturography (CDP) vestibular training program combined with home-based exercises designed to improve balance function and reduce the risk of falling by an individual with a posterior fossa tumor.
CASE REPORT: A 36-year-old male patient was diagnosed with dysplastic gangliocytoma/ganglioglioma according to magnetic resonance imaging, computed tomography, and pathology reports on March 28, 2016. The patient was treated by partial cerebellar tumor resection on April 7, 2016. After the operation, he reported severe imbalance, nausea, and vomiting for 1 month and visited the Audiology Department on October 20, 2016. The patient was evaluated with the CDP-sensory organization test (SOT) and his composite equilibrium score of this examination was 48, 31% below normal. We administered a 6-week posturography-assisted vestibular rehabilitation (VR) protocol (extending an hour per week) combined with a home-based exercise program twice in 2 years. In the second evaluation we applied in 2018, SOT composite equilibrium score increased to 72 after VR, reaching normal limits. After 2 years, his complaints slightly alleviated and his SOT scores were better when we compared the VR results in 2016.
CONCLUSIONS: We demonstrated that long-term VR may affect a patient with dysplastic cerebellar gangliocytoma (LDD) presenting imbalance or dizziness.
Keywords: Hamartoma Syndrome, Multiple, Physical and Rehabilitation Medicine, Vestibular Function Tests, Cerebellar Neoplasms, Cerebellum, Child, Follow-Up Studies, Ganglioneuroma, Magnetic Resonance Imaging
Background
Lhermitte-Duclos disease (LDD), or dysplastic gangliocytoma of the cerebellum, is a congenital malformation characterized by a slow-growing unilateral cerebellar mass, usually presenting in the posterior fossa [1,2]. Dysplastic cerebellar gangliocytoma is seen most frequently in the third or fourth decade [3]. Tumors that affect the midbrain, cerebellum, and brain stem may disrupt visual fixation and vestibular and gaze-stabilization mechanisms, which can lead to acquired nystagmus, skew deviation, complex gaze palsies, positional vertigo, dis-equilibrium, and headaches [4,5]. However, more commonly, the patient experiences disequilibrium that they cannot explain and that occurs gradually over time as the tumor infiltrates or compresses the vestibular nerve [5]. Vestibular rehabilitation (VR) is a customized form of rehabilitation using activities and movement with home-based computer-assisted exercises that provide ability to maintain gaze stability, balance, and sensory organization. Studies have shown that VR is effective in patients with both central and peripheral vestibular dysfunction [6,7].
Case Report
A 36-year-old male patient underwent excision of the cerebellar tumor on April 7, 2016 as he was diagnosed with dysplastic gangliocytoma/ganglioglioma (Figure 1). Preoperative magnetic resonance imaging (MRI) showed a mass in the right cerebellum, which is mixed hyperintense on T2 weighted image. The patient’s postoperative MRI scan showed that the patient’s vermis superior had a stable residual tumor, and right cerebellum inferior and vermis uvula showed volume loss after the operation (Figure 2). The patient had difficulties in walking, blurred vision, tinnitus, diplopia, and dizziness before surgery related to the tumoral pathology. After the operation, he reported severe imbalance, nausea, and vomiting for 1 month. For this reason, the patient was sent to our clinic by the Neurology Department on October 20, 2016. Vestibular evaluation results in the Audiology Department shown that the patient had difficulties in walking, disturbed control of the center of gravity (COG), and had problem with losing sensation while walking up the stairs. In addition, the patient’s pure tone average was within the normal range but his audiogram configuration showed bilaterally a slope toward high frequencies.
A typical bedside screening test consisting of multiple measures to evaluate ocular motor control, vestibulo-ocular reflex (VOR), and vestibulospinal reflex function was applied. Bedside tests were combined with videonystagmography (VNG) and other tests to support the result during laboratory investigation.
Balance-related outcome measures were completed as follows: 1) computerized testing with the sensory organization test (SOT), limits-of-stability test, and adaptation test on the NeuroCom EquiTest® computerized dynamic posturography (CDP) system. NeuroCom’s EquiTest CDP system is an assessment technique to quantify and differentiate the sensory, motor, and central adaptive impairments in balance control.
According to results obtained from examination on October 20, 2016, Romberg and tandem Romberg tests were positive and during the Unterberger test (Fukuda stepping test) the patient veered to the right and showed a bilateral tendency to fall during a straight-line walking test (open and closed eyes). According to the VNG test battery, in the head-shake test, we obtained 10° downbeat nystagmus. Pursuit and optokinetic tests showed low gain. Additionally, hypermetric saccades (overshoots) were observed in the saccade-random test. There was strong evidence in the findings of VNG regarding the fact that the patient was affected by central vestibular pathology (Table 1). No bilateral ocular-vestibular-evoked myogenic potentials (VEMP) response was observed, whereas bilateral cervical VEMP was observed, and there was no asymmetry in responses.
Utilizing CDP, the patient’s composite equilibrium score was obtained as 48 in SOT. Moreover, SOT results revealed difficulties with conditions 5 and 6. The patient was mostly dependent on somatosensory information for balance. Visual and vestibular response scores were also below the normal range in sensory analysis testing. Strategy analysis and the COG alignments were within a normal range (Figure 3).
The patient was at risk of falling as indicated by a score of 40/56 on the Berg balance scale (BBS) and he was also at risk of falling as indicated by SOT composite equilibrium score on the CDP. Therefore, we decided to include the patient in the VR program. A signed consent form was obtained.
In December 2016, a 6-week home-based posturography-assisted rehabilitation program ended with improvement of the patient’s gaze stability, decreasing postural sway, and risk of falling (Figure 3). At the end of the rehabilitation program, his composite equilibrium score increased to 66.
In 2017, the patient was unable to be admitted to the hospital because of his expired health insurance. Therefore, the patient could not be followed up during 2017. In 2018, the patient was evaluated at the Hospital Vertigo Council, so the case was reanalyzed. For this reason, the patient underwent an audiological examination in our clinic on October 31, 2018. At this time, we administered the same examination protocol for the follow-up case. During this period, the patient reported difficulty in walking and balance. In oculomotor tests, we observed pathological findings similar to those in 2016 (Table 1). The patient’s video head impulse test (VHIT) was obtained within the normal gain range. (Figure 4).
CDP-SOT findings revealed that the patient still had difficulties in 5th and 6th conditions. In sensory analysis, even if the visual component improved, findings showed poor performance in the vestibular component. Strategy analysis results showed that the patient was dependent on the ankle strategy. His composite equilibrium score was 63 in SOT (Figure 5).
At follow-up in 2018, we observed that the patient improved slightly but still had imbalance and difficulties while walking. Because of the patient’s ongoing complaints and test findings, a modified VR program was planned.
The program we applied to the patient twice in 2 years consisted of vestibular adaptation exercises, habituation exercises, balance/gait activities, and general fitness training (Cawthorne-Cooksey, rhythmic-weight-shift test [RWS], four-corners step test [FCS], and stand: marching in place test [SMP]). RWS, SMP, and FCS tests were applied to the patient via CDP. The RWS test measures the patient’s ability to voluntarily move his COG or sway horizontally or anteriorly/posteriorly in a rhythmic manner between 2 targets [8]. The FCS is a dynamic test that measures the ability to rapidly cross over obstacles and change direction via CDP [9]. First, a fixed supporting surface and surroundings were used in the tests, and then mobility of the supporting surface and surroundings were gradually increased. Our aim here was to force the patient to use his vestibular sensation more than proprioceptive and visual senses for balance.
According to the test results of our patient on November 2, 2018, VR training was given. Mobility training tasks such as SMP and FCS were performed because of the patient’s complaints about his movement on stairs. These activities were multiplied systematically according to scores obtained by the patient during treatment sessions. Tasks were repeated during each session with a higher level of difficulty or replaced with more advanced training (Table 2).
After a 6-week rehabilitation program, the patient’s complaints decreased slightly and his composite equilibrium score was 72. In addition, visual and vestibular responses were within a normal range of sensory analysis and strategy analysis. The COG alignments were within normal range (Figure 5). The patient’s BBS score increased from 40/56 (in 2016) to 49/56 (in 2018). SOT and BBS results showed that the patient’s risk of falling was eliminated. The patient reported that his life quality improved in general.
Discussion
In this case report, we described a CDP-assisted VR protocol combined with a home-based exercise program approach that addresses challenges of body stability in standing and walking. Robinson and Cohen determined that there are only 220 diagnosed cases of LDD [10]. However, there is no study that shows that LDD patients undergo VR. This case report is the first study to demonstrate that long-term VR has efficacy for a patient with partial cerebellum tumor excision.
This study suggests that exercises that activate postural and neural control mechanisms in the treatment program may be more effective in maintaining posture and coordination of sequential movements. This kind of mechanism may involve integration of sensory information or motor control strategies to increase postural and gaze stability [11,12]. We reported the patient’s response to treatment in terms of clinical balance assessment and whole-body motion analysis via computerized posturography.
CDP can objectively assess changes in vestibular impairments and has been broadly used clinically for about 30 years to test balance. Although posturography-assisted rehabilitation utilizing visual feedback seems to improve postural control, little is known about its usefulness in rehabilitation programs, especially for patients with central vestibular disorders (CVD) [13].
Brown et al. [14] evaluated 48 CVD patients with a balance scale and questionnaire tests, which included emotional, physical, and functional states. These tests consisted of activities-specific balance confidence scale, the dizziness handicap inventory, the dynamic gait index, and the timed up & go test. In evaluation of the whole group, significant differences were demonstrated between baseline assessment and discharge [14]. Bittar and Barros prospectively considered 8 patients with CVD who were treated with electric stimulation; although three-quarters of patients reported being more stable, there was no improvement in balance control in CDP [15].
Literature to support the use of VR in the treatment of CVD is insufficient. Hence, less is known about the efficacy of VR with CVD such as multiple sclerosis, brain tumors, cerebellum lesion, or disease [16]. Many aspects of VR are similar for patients with CVD and peripheral vestibular disorders (PVD). However, studies demonstrate that people with CVD have poorer outcomes and do not progress as promptly when compared with those with PVD [16].
The cerebellum plays an important role in control of eye movements, physical movement and coordination, and cognitive processes. The sections of the cerebellum are functionally divided into 3 groups: vestibulocerebellum (flocculus, paraflocculus, nodulus, uvula, tonsil, and cerebellar pyramid), spinocerebellum (vermis and the intermediate zones of the cerebellar cortex, as well as the fastigial and interposed nuclei), and cerebro-cerebellum. Lesions of vestibulocerebellar, vestibulospinal, or cerebellar oculomotor systems can lead to vertigo, dizziness, and imbalance [17]. The cerebellum controls calibration, eye stability, gaze-holding processing, and inhibition of undesirable saccades [18].
Ocular instability, nystagmus, saccadic intrusions, impaired smooth pursuit, impaired VOR, and ocular misalignment may occur in cerebellar dysfunction [17]. Abnormal findings in the patient’s oculomotor tests (Table 1), poor postural control (Figures 3A, 5A), difficulty in walking, and symptoms of hypotonia and chronic imbalance show structural-clinical correlations according to the regions where the tumor and surgery anatomically affect the cerebellum of the patient.
Cerebellar lesions may have different effects on VOR. Halmagyi et al. [19] stated that the function of VOR in cerebellar lesions is related to degeneration of the flocculus and vestibular nucleus. They also reported that in patients with partial cerebellar lesions, nondamaged regions of the cerebellum can participate in learning and adaptation [19]. VHIT findings of our patient may have been related to this condition.
Gill-Body et al. [20] examined 2 patients with cerebellar pathology (cerebellar tumor and cerebellar atrophy). These patients performed eye-coordination exercises, balance stabilization, and walking activities. They reported that rehabilitation was important when the cerebellum was not completely lost, as postural stability improved significantly as a result of exercises [20].
In addition, Gill-Body et al. achieved successful results by applying rehabilitation programs including Frenkel exercises and balance/walking activities in patients with cerebellar dysfunction. This indicates that improvement of vestibular dysfunction may be possible even after cerebellar lesions [20]. They also stated that possible healing mechanisms such as neural attraction, plasticity, and substitution [20,21] are occurring.
The purpose of rehabilitation in our case with LDD was to try to recover postural stability when central nervous system structures were damaged. Probably one of the most challenging cases are those with CVD. Therefore, effects of VR often occur slowly and observed benefits are delayed because of the damage of the involvement of the central vestibular components responsible for compensation [22].
Conclusions
This is a rare case report that demonstrates that even a 36-year-old adult with partial excision of the cerebellum may benefit from long-term VR. Although the cerebellum is an important part of the balance system and compensation mechanism, even patients who have undergone a partial excision of the cerebellum may be candidates for a VR program. More research is needed to investigate its effectiveness for patients with cerebellar pathology and to better understand the strategies used by people with balance disorders to increase their postural control and gaze stability.
Figures
References:
1.. Andres RH, Guzman R, Weis J, Lhermitte-Duclos disease with atypical vascularisation – Case report and review of the literature: Clin Neuropathol, 2009; 28; 83-90
2.. Izukawa D, Lach B, Benoit B, Gangliocytoma of the cerebellum: Ultrastructure and immunohistochemistry: Neurosurgery, 1988; 22(3); 576-81
3.. Shinagare AB, Patil NK, Sorte SZ, Case 144: Dysplastic cerebellar gangliocytoma (Lhermitte-Duclos disease): Radiology, 2009; 251(1); 298-303
4.. Gadgil N, Edmond J, Stormes K, Visual complications of pediatric posterior fossa tumors: Analysis of outcomes: Pediatr Neurol, 2019; 92; 48-54
5.. Weber PC: Vertigo and disequilibrium: A practical guide to diagnosis and management, 2017, New York, Thieme Publishers
6.. Balci BD, Akdal G, Yaka E, Angin S, Vestibular rehabilitation in acute central vestibulopathy: A randomized controlled trial: J Vestib Res, 2013; 23(4–5); 259-67
7.. McDonnell MN, Hillier SL, Vestibular rehabilitation for unilateral peripheral vestibular dysfunction: Cochrane Database Syst Rev, 2015; 1; CD005397
8.. Nallegowda M, Singh U, Bhan S, Balance and gait in total hip replacement: A pilot study: Am J Phys Med Rehabil, 2003; 82(9); 669-77
9.. Dite W, Temple VA, A clinical test of stepping and change of direction to identify multiple falling older adults: Arch Phys Med Rehabil, 2002; 83(11); 1566-71
10.. Robinson S, Cohen AR, Cowden disease and Lhermitte-Duclos disease: An update. Case report and review of the literature: Neurosurg Focus, 2006; 20(1); E6
11.. Balliet R, Harbst KB, Kim D, Stewart RV, Retraining of functional gait through the reduction of upper extremity weight-bearing in chronic cerebellar ataxia: Int Rehabil Med, 1987; 8(4); 148-53
12.. Shumway-Cook A, Woolacott MH, Assessment and treatment of patients with postural disorders: Motor Control: Theory and Applications, 1995; 207-35, Baltimore, Md, Williams & Wilkins
13.. Cakrt O, Chovanec M, Funda T, Exercise with visual feedback improves postural stability after vestibular schwannoma surgery: Eur Arch Otorhinolaryngol, 2010; 267(9); 1355-60
14.. Brown KE, Whitney SL, Marchetti GF, Physical therapy for central vestibular dysfunction: Arch Phys Med Rehabil, 2006; 87(1); 76-81
15.. Bittar RS, de Giacomo Carneiro Barros C, Vestibular rehabilitation with biofeedback in patients with central imbalance: Braz J Otorhinolaryngol, 2011; 77(3); 356-61
16.. Furman JM, Whitney SL, Central causes of dizziness: Phys Ther, 2000; 80(2); 179-87
17.. Bodranghien F, Bastian A, Casali C, Consensus paper: Revisiting the symptoms and signs of cerebellar syndrome: Cerebellum, 2016; 15(3); 369-91
18.. Manto M, Bower JM, Conforto AB, Consensus paper: Roles of the cerebellum in motor control-the diversity of ideas on cerebellar involvement in movement: Cerebellum, 2012; 11(2); 457-87
19.. Halmagyi GM, Chen L, MacDougall HG, The video head impulse test: Front Neurol, 2017; 8; 258
20.. Gill-Body KM, Popat RA, Parker SW, Krebs DE, Rehabilitation of balance in two patients with cerebellar dysfunction: Phys Ther, 1997; 77(5); 534-52
21.. Amici R, Avanzini G, Pacini L, Cerebellar tumors. Clinical analysis and physiopathologic correlations: Monogr Neural Sci, 1976; 4; 1-112
22.. Suarez H, Arocena M, Suarez A, Changes in postural control parameters after vestibular rehabilitation in patients with central vestibular disorders: Acta Otolaryngol, 2003; 123(2); 143-47
Figures
Tables
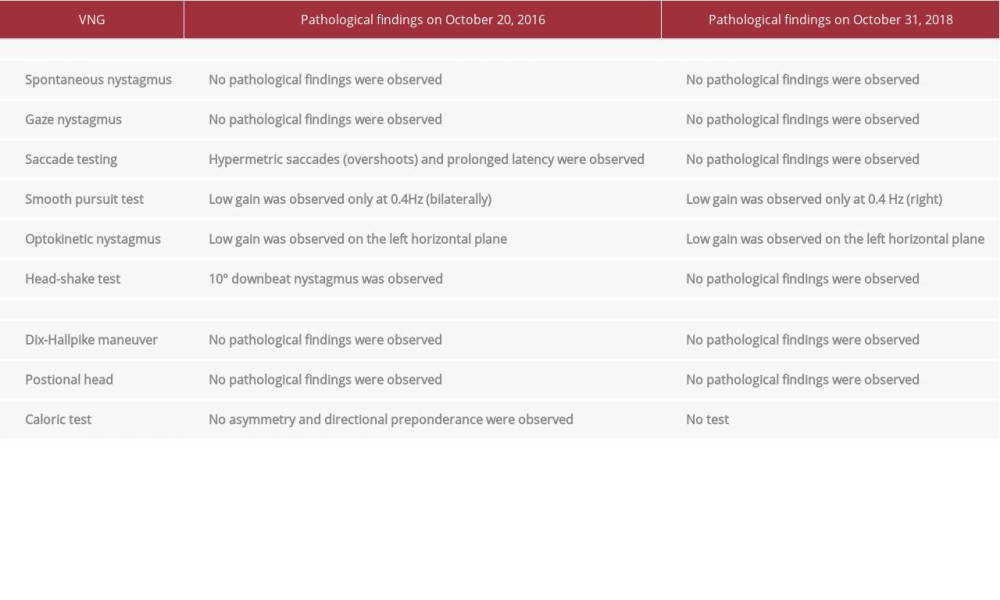 Table 1.. The patient’s videonystagmography (VNG) findings.
Table 1.. The patient’s videonystagmography (VNG) findings. Table 2.. Exercise programs (adaptation, habituation, substitution) against problem areas of the patient who had cerebellum excision.
Table 2.. Exercise programs (adaptation, habituation, substitution) against problem areas of the patient who had cerebellum excision.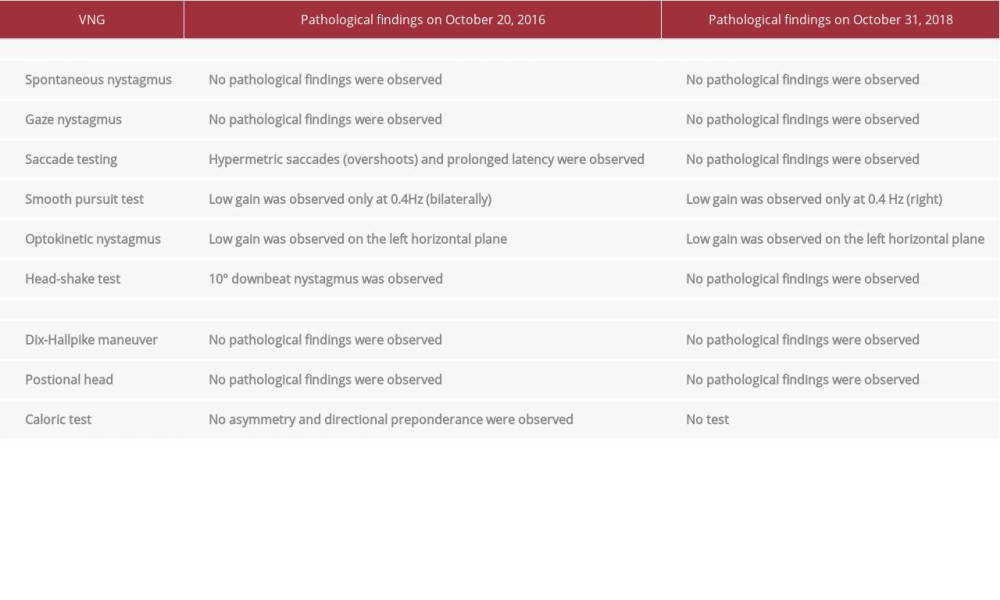 Table 1.. The patient’s videonystagmography (VNG) findings.
Table 1.. The patient’s videonystagmography (VNG) findings. Table 2.. Exercise programs (adaptation, habituation, substitution) against problem areas of the patient who had cerebellum excision.
Table 2.. Exercise programs (adaptation, habituation, substitution) against problem areas of the patient who had cerebellum excision. In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








