23 January 2021: Articles 
A Case of Adrenal Insufficiency Diagnosed Using Optimal Dosing of Cosyntropin During Stimulation Testing
Unusual clinical course, Mistake in diagnosis, Diagnostic / therapeutic accidents, Educational Purpose (only if useful for a systematic review or synthesis)
Clio Musurakis1DEF*, Solab Chitrakar1DEF, Ekta Shrestha1DEF, Randa Sharag Eldin2DEF, Mariam Charkviani1DEF, Gauri Pethe1DEF, Faisal Qureshi3DEFDOI: 10.12659/AJCR.927533
Am J Case Rep 2021; 22:e927533
Abstract
BACKGROUND: This case report illustrates the difficulties that arise during diagnosis of adrenal insufficiency, especially in the general medicine setting. Symptoms can often be nonspecific, and when a serum cortisol level is checked, further difficulty exists as to how to interpret the results. The 250-μg cosyntropin dose or 1-μg dose are available for use in the diagnosis of adrenal insufficiency, but each test has its own indications, which will be discussed.
CASE REPORT: A 45-year-old woman presented with nausea, emesis, chills, and diaphoresis, symptoms that concerning for adrenal insufficiency. Her random serum cortisol levels were relatively low. Her ACTH levels were within normal range. She received additional testing with the ACTH stimulation test using both the 1-μg and the 250-μg dose. The 1-μg test was performed in the evening and showed an inadequate adrenal response. The 250-μg dose test, which is the criterion standard, was performed the following morning and excluded adrenal insufficiency.
CONCLUSIONS: With the use of the high-dose ACTH stimulation test performed in the early morning, this patient was able to avoid lifelong steroid replacement therapy that could potentially suppress the hypothalamic-pituitary-adrenal (HPA) axis, which of itself can lead to adrenal insufficiency. Careful consideration is needed in choosing the right modalities for diagnosis of adrenal insufficiency.
Keywords: adrenal insufficiency, Adrenocorticotropic Hormone, corticotropin-releasing hormone, Cosyntropin, Hydrocortisone, Hypothalamo-Hypophyseal System, Pituitary-Adrenal System
Background
Symptoms of adrenal insufficiency can often be nonspecific, and the diagnosis may sometimes elude physicians until adrenal crisis occurs. However, when serum cortisol level is checked, further difficulty exists regarding how to interpret the results. The adrenocorticotropic hormone (ACTH) test, also referred to as the cosyntropin stimulation test, is then used to further categorize the patient as adrenally “sufficient” or “insufficient.” Careful selection of the ACTH dose is required to yield an appropriate adrenal response. The use of the 250-μg cosyntropin dose test, also referred to as the high-dose ACTH test, is the criterion standard test for diagnosis of primary adrenal insufficiency. The 1-μg dose test, also referred to as the low-dose test, is mostly reserved for diagnosis of secondary adrenal insufficiency. Both tests should be performed in the early morning. Careful consideration of the results produced during the diagnostic process is imperative to avoid mislabeling of patients with a disease that requires lifelong treatment.
Case Report
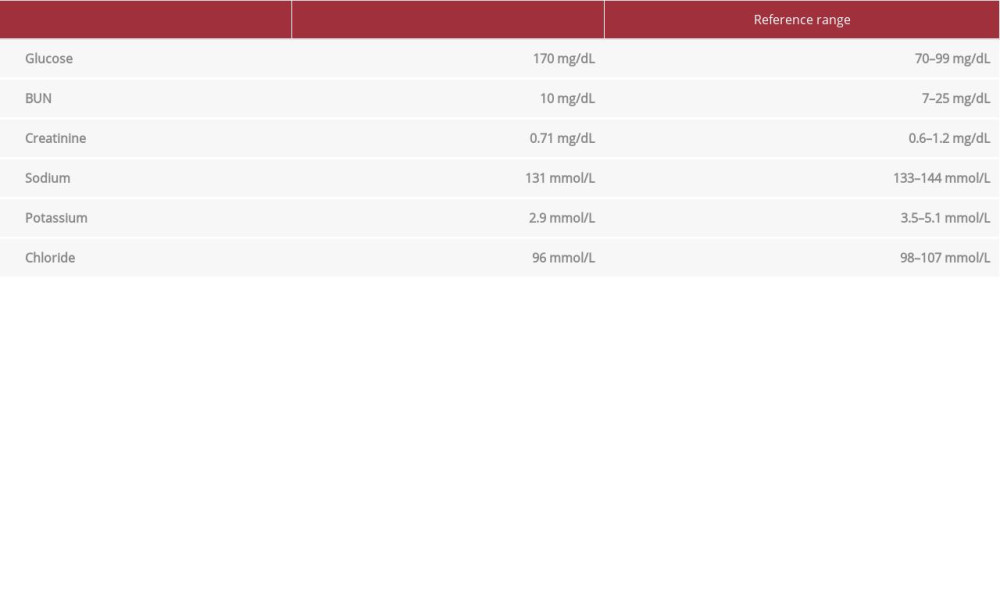
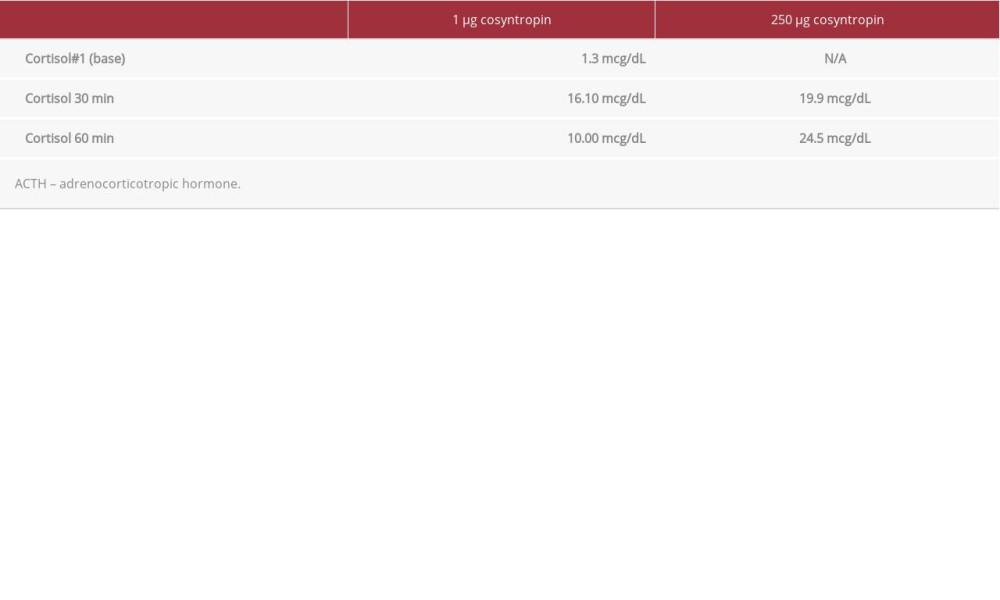
We report the case of a 45-year-old woman with a history of asthma and psoriasis who presented with emesis. Home medications included monthly TNF-alpha inhibitor injections for psoriasis, triamcinolone acetonide topical spray, and budesonideformoterol inhaler. The use of inhaled steroids was inconsistent and infrequent, as was the use of the steroid spray. She started the TNF-alpha inhibitor injections a few months before presentation. The patient reported increased urinary frequency with no dysuria and excessive water intake for 2 days prior to presentation. On the day of admission, she started having nausea, chills, and diaphoresis while at work, followed by 2 episodes of nonbloody nonbilious emesis. She also had associated palpitations, lightheadedness, leg cramps, and shortness of breath. She had no chest pain. When she arrived at the emergency room, she had blood pressure of 107/59 mmHg, heart rate of 89 beats/min, respiratory rate of 16 breaths/min, temperature of 36.5°C and oxygen saturation of 98% on room air. Her physical exam revealed cold, clammy distal extremities but was otherwise unremarkable. A work-up was negative for human chorionic gonadotropin (hCG), high-sensitivity troponin, d-dimer, urine drug toxicology, lipase, blood alcohol level, and acetaminophen level. A complete blood count (CBC) was unremarkable. Results of a comprehensive metabolic panel were concerning for anion gap metabolic acidosis, hyponatremia, and hypokalemia (Table 1). Magnesium and TSH were within normal range. She was treated with intravenous potassium and albuterol nebulizer. Her laboratory results returned normal the following day, except for a random serum cortisol of 6.4 mcg/dL. ACTH was 7 pg/dL (reference range 6–58 pg/mL). Due to concern for adrenal insufficiency, a 1-μg cosyntropin test was performed in the evening, which showed a peak cortisol concentration of less than 18 mcg/dL. As the response was assessed as suboptimal, Endocrinology was consulted to offer a treatment plan for steroids. However, it was discovered then that the use of 1-μg cosyntropin was unintentional and the timing of performance was inappropriate, as this should have been performed in the early morning. Once this was recognized, the test was repeated the following morning using the criterion standard 250-μg cosyntropin dose. The patient then showed an adequate response and she was not started on steroids.
Discussion
Thomas Addison was the first to describe adrenal insufficiency (AI) in 1855. It can either be of primary etiology when adrenal glands fail to produce hormones, or of central etiology when the pituitary gland or hypothalamus fail to produce releasing hormones that activate adrenal hormone production. Commonly described symptoms include fatigue, weakness, anorexia, abdominal pain, weight loss, orthostatic hypotension, and salt craving. Characteristic hyperpigmentation of the skin is seen with primary adrenal failure [1]. Since symptoms are nonspecific, it is generally difficult for physicians to diagnose AI; most patients present to providers with symptoms of adrenal insufficiency 3 of 4 times before a correct diagnosis is made. The timing of serum cortisol sampling can also affect diagnosis, since secretion depends on the circadian rhythm and on the state of health. Generally, a random serum cortisol of over 14.5 mcg/dL (or 400 nmol/L) at any time of the day makes adrenal insufficiency highly unlikely, while a morning serum cortisol of less than 3.6 mcg/dL (or 100 nmol/L) strongly suggests adrenal failure [2]. Our patient’s cortisol level was 6.4 mcg/dL, and adrenal insufficiency could not be excluded with this test result alone.
The ACTH stimulation test is used when serum cortisol levels cannot provide a certain diagnosis. In this test, 250 μg of intravenous synthetic ACTH is given to the patient and serum cortisol is measured 30 and 60 min later. Cortisol values exceeding 18 to 20 mcg/dL either at the 30- or 60-min mark usually represent a normal response [3]. This test should be performed when cortisol levels are 3–15 mcg/dL, as was the case with our patient. It cannot be used to diagnose secondary adrenal insufficiency of recent onset (within 4–6 weeks), as the adrenal glands are not completely atrophic yet and are still producing cortisol, as in pituitary apoplexy or recent pituitary surgery [4]. If testing occurs when the patient is acutely ill, the test should be repeated at a later date [2]. In our case, the patient exhibited low random cortisol levels, likely in the setting of acute illness (hypokalemia, asthma exacerbation), which prompted more investigation with an ACTH stimulation test (see comparison in Table 2). Instead of the criterion standard 250-μg ACTH stimulation test, a 1-μg test was ordered. Some suggest that the 1-mcg test can be used for diagnosis of primary AI and this is often done in clinical practice, but the 250-mcg test is the criterion standard for diagnosis according to the Endocrine Society guidelines [5]. There is concern that the 250-mcg test may lead to supraphysiologic stimulation of the HPA axis and false-positive results [6]. However, others argue that the 1-mcg test carries the risk of mislabeling healthy individuals as adrenally insufficient [7]. According to the Endocrine Society guidelines, the 1-mcg test should be used only when cosyntropin is in short supply, as this test has not been validated yet and more studies are needed to compare it to the 250-mcg test [5,6].
There are instances when the 1 mcg ACTH stim test can be used to screen for disturbances of the hypothalamo-pituitary-adrenocortical axis. The 1-μg ACTH stimulation test has been shown to be more sensitive than the 250-μg test in diagnosing secondary adrenal insufficiency [8]. Our patient, however, had a normal ACTH level (7 pg/dL, with a reference range of 6–58 pg/mL); therefore, the use of a 250-μg test was most appropriate according to current guidelines [5]. The 1-μg test has also been shown to be superior in diagnosing adrenal insufficiency in critically ill ICU patients, although more studies are needed to validate this [3].
Chronic use of glucocorticoids can lead to adverse effects such as cardiovascular disease, hyperglycemia, infections, osteoporosis, neuropsychiatric events, and growth failure in children [9].
Gastrointestinal, ophthalmologic, and dermatologic disturbances are common as well [10]. Steroids exert negative feedback control on the HPA axis by suppressing the hypothalamus which produces corticotropin-releasing hormone (CRH) and the pituitary gland which produces ACTH. Since the adrenal glands are not stimulated anymore by the released hormones to produce cortisol, the result of chronic suppression is adrenal atrophy, especially when using high-dose steroids [9]. In our case, the long-term administration of steroid therapy to the patient was avoided with careful review of the diagnostic process and patient history, which prevented the development of all the above-mentioned adverse effects to an otherwise healthy individual.
It is important to note that steroid doses equivalent to 7.5 mg of prednisolone taken for 3 weeks or longer can lead to adrenal suppression. However, it has been found that people taking medications that reduce steroid metabolism (e.g., potent CYP3A4 inhibitors) can develop HPA axis suppression with co-administration of even small doses of exogenous steroid (typically, inhaled fluticasone) [2]. Our patient was not on any CYP3A4 inhibitors and her sporadic use of topical and inhaled steroid was very unlikely to have caused secondary AI due to withdrawal of medications.
Conclusions
This case demonstrates how the 250-μg ACTH (high-dose) stimulation test should be used for diagnosis of primary adrenal insufficiency (AI), as it is still the criterion standard. The 1-μg ACTH (low-dose) stimulation test can be used for diagnosis of primary AI, but only when the high-dose test is not available. On the other hand, the 1-μg ACTH stimulation test has been shown to be more sensitive than the 250-μg test in diagnosing secondary adrenal insufficiency. Both tests should be performed in the early morning. The clinician can offer the patient the best treatment strategies only after correctly using the most appropriate test. Our patient was an adrenally “sufficient” individual who did not require chronic replacement therapy. The steroids in this case could have harmed the patient, as long-term administration of this unnecessary medicine would have carried a multitude of adverse effects, including the risk of adrenal gland suppression. If further diagnostic difficulty exists, testing can always be repeated at a later date.
References:
1.. Charmandari E, Nicolaides NC, Chrousos GP, Adrenal insufficiency: Lancet, 2014; 383(9935); 2152-67
2.. Pazderska A, Pearce SH, Adrenal insufficiency – recognition and management: Clin Med (Lond), 2017; 17(3); 258-62
3.. Hamilton DD, Cotton BA, Cosyntropin as a diagnostic agent in the screening of patients for adrenocortical insufficiency: Clin Pharmacol, 2010; 2; 77-82
4.. Alexandraki KI, Grossman A: Adrenal Insufficiency, 2000, Endotext South Dartmouth (MA), MDTextcom, Inc https://www.ncbi.nlm.nih.gov/sites/books/NBK279122/
5.. Bornstein SR, Allolio B, Arlt W, Diagnosis and treatment of primary adrenal insufficiency: An endocrine society clinical practice guideline: J Clin Endocrinol Metab, 2016; 101(2); 364-89
6.. Mongioì LM, Condorelli RA, Barbagallo F, Accuracy of the low-dose ACTH stimulation test for adrenal insufficiency diagnosis: A re-assessment of the cut-off value: J Clin Med, 2019; 8(6); 806
7.. Abdu T, Clayton R, The low-dose Synacthen test for the assessment of secondary adrenal insufficiency: Current Opinion in Endocrinology & Diabetes, 2000; 7; 116-21
8.. Talwar V, Lodha S, Dash RJ, Assessing the hypothalamo-pituitary-adrenocortical axis using physiological doses of adrenocorticotropic hormone: QJM, 1998; 91(4); 285-90
9.. Nicolaides NC, Pavlaki AN, Maria Alexandra MA, Chrousos GP: Glucocorticoid therapy and adrenal suppression, 2018, Endotext South Dartmouth (MA), MDTextcom, Inc
10.. Yasir M, Goyal A, Bansal P, Sonthalia S: Corticosteroid adverse effects, 2020, Treasure Island (FL), StatPearls Publishing
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250