13 March 2021: Articles 
Immunodeficiency and Thymoma: A Case Report on Good Syndrome, a Diagnosis Frequently Missed and Forgotten
Challenging differential diagnosis, Unusual setting of medical care, Rare disease
Andy Sing Ong Tang1ABCDEF*, Wei Huei Loh2BCEF, Qi Ying Wong2BCDEF, Siaw Tze Yeo2BCDEF, Wei Loon Ng3BDF, Pak Inn Teoh4BD, Tem Lom Fam1BDEG, Lee Ping Chew5ABDEF, Hock Hin Chua6ADEFDOI: 10.12659/AJCR.928659
Am J Case Rep 2021; 22:e928659
Abstract
BACKGROUND: Good syndrome (thymoma with immunodeficiency) is a frequently missed and forgotten entity. It is a rare cause of combined B and T cell immunodeficiency in adults. To date, fewer than 200 patients with Good syndrome have been reported in the literature.
CASE REPORT: We report a case of type AB Masaoka-Koga stage I thymoma which predated the evidence of immune dysregulation by 5 years, manifesting as bilateral cytomegalovirus retinitis, multiple bouts of pneumonia, and bronchiectasis in a HIV-seronegative 55-year-old man. Intravitreal ganciclovir was administered in addition to intravenous systemic ganciclovir, which resulted in severe neutropenic sepsis. A thorough immunodeficiency workup confirmed the presence of hypogammaglobulinemia with complete absence of B cells and reduced CD4/CD8 ratio. The patient responded well to monthly intravenous immunoglobulin replacement therapy, with no further episodes of infection since then. The immunoglobulin level doubled after 1 year of treatment. However, as the patient refused further intravitreal and CMV-targeted treatment, his vision did not recover.
CONCLUSIONS: Clinicians should be aware that thymoma can precede the onset of immunodeficiency. Clinical suspicion should be heightened in at-risk patients who present with multiple bouts of infection, particularly in thymoma cases with adult-onset immune dysfunction. It is of paramount importance to follow up those patients with annual clinical reviews and immunodeficiency screening.
Keywords: Agammaglobulinemia, Cytomegalovirus Retinitis, Thymoma, Immunoglobulins, Intravenous, Thymus Neoplasms
Background
Good syndrome (GS), with the reported incidence of 0.15 cases per 100 000 population per year, is a rare and frequently forgotten adult-onset immunodeficiency disorder in association with the presence of thymoma [1]. To date, fewer than 200 patients with GS have been reported in the literature. We present a case of thymoma which preceded the evidence of immunodeficiency, manifesting as frequent bouts of infection.
Case Report
A 55-year-old eman who was previously healthy was found to have a widening anterior mediastinal mass on chest X-ray (CXR) during pre-employment health screening in 2014. He underwent thymectomy in which the histopathological examination (Figure 1) showed type AB Masaoka-Koga stage I thymoma (well-differentiated, non-invasive subtype) which warranted complete surgical excision without necessitating postoperative radio-chemotherapy. He was then followed up annually, during which his clinical symptoms and signs were reviewed in addition to laboratory (full blood count and inflammatory markers) and radiological (computed tomography [CT] thorax) investigations. He was a non-smoker and non-drinker with no prior medical illnesses or high-risk behaviors.
Five years later, he presented with chronic productive cough, several bouts of pneumonia, and blurring of vision in both eyes. He denied altered mental status, hemoptysis, gastrointestinal symptoms, skin lesions, and constitutional symptoms like night sweats and loss of appetite. No tuberculosis (TB) exposure was identified. On examination, the visual acuity of both eyes was counting fingers (right) and 6/24 (left). Anterior segments were unremarkable. Fundus examination showed bilateral retinitis mixed with retinal hemorrhage in pizza-pie appearance at the posterior pole (Figure 2). The optic discs were normal. There was no clinical evidence of post-thymectomy myasthenia gravis.
Investigations showed a positive IgG cytomegalovirus (CMV) serology, with negative IgM CMV, toxoplasma, and rubella and herpes simplex virus (HSV) serology. His serum CMV polymerase chain reaction (PCR) result was 2545 IU/ml. He was seronegative for syphilis, hepatitis B/C, and HIV. Sputum acid-fast bacilli (AFB), cultures for bacteria, fungal, and mycobacterium, as well as tuberculosis PCR, were negative. Autoimmune screening (antinuclear antibody, C3, C4) was negative. The annual computed tomography (CT) thorax (as part of thymoma surveillance) demonstrated presence of tree-in-bud and bronchiectasis changes, without evidence of recurrence. A diagnosis of bilateral CMV retinitis was made based on clinical features of his eyes, in correlation with his background history of thymoma. Intravitreal ganciclovir (2 mg each eye, twice a week) was administered in addition to intravenous systemic ganciclovir (5 mg/kg twice daily) in view of the involvement of zone I at the posterior pole. Unfortunately, he developed severe neutropenic sepsis complicated by pneumonia after 4 days of intravenous ganciclovir, whereby his absolute lymphocyte count (ALC) reached a nadir of 0.41×103/µL, in comparison with ALC value (1.3×103/µL) before the onset of CMV disease.
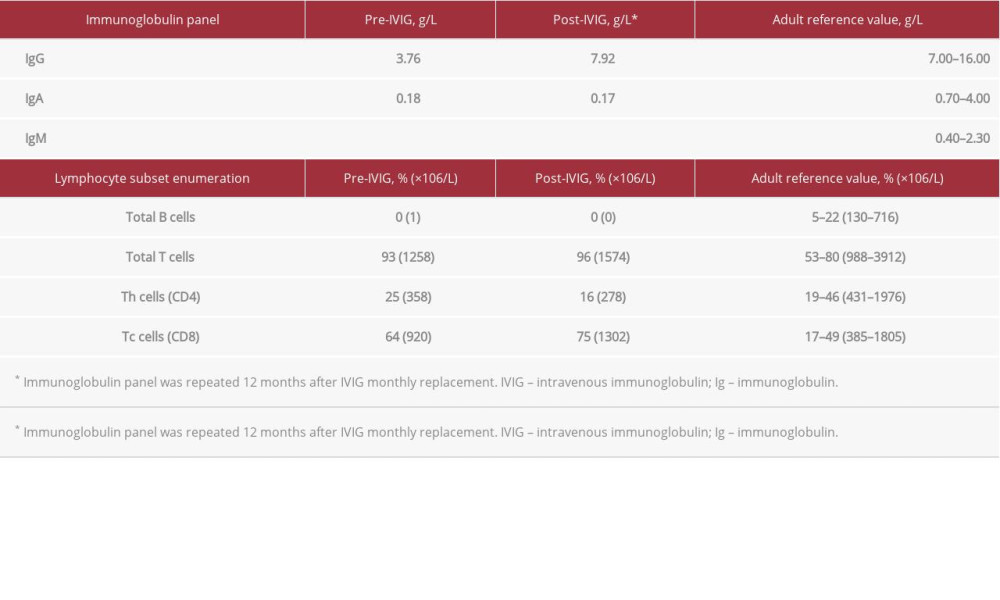
Immunodeficiency workup was performed, which included flow cytometric lymphocyte subset enumeration and quantitation of immunoglobulin (Table 1). He was found to have complete absence of B cells and evidence of hypogammaglobulinemia with reduced CD4/CD8 ratio (0.39). The overall clinical manifestations and laboratory findings were consistent with the diagnosis of Good syndrome in association with thymoma, complicated by CMV retinitis and pneumonia resulting in bronchiectasis.
The patient was started on intravenous immunoglobulin (IVIG) replacement therapy (0.4 g/kg monthly) up to date without other medications. No further episodes of infection were found after the initiation of IVIG treatment. His IgG level had doubled after 1 year of IVIG therapy (Table 1). However, he refused further intravitreal and CMV-targeted treatment despite multiple counseling sessions involving the multidisciplinary team, as he attributed his bad experience to the adverse effects of ganciclovir. The retinitis patch eventually turned into retinal scars involving the macula, therefore, vision was poor in both eyes (counting fingers).
Discussion
The detection of thymoma, which is a malignant epithelial neoplasm that arises from the thymus, is reported to predate immunodeficiency in about half of patients [2]. This is in accordance with our patient, whose immune dysfunction was evidenced by clinical manifestation of frequent infections 5 years after the finding of thymoma.
GS differs from common variable immune deficiency (CVID) and X-linked agammaglobulinemia (XLA) in terms of its very late onset, lack of familial cases, and absence of lymphoid hyperplasia [3]. This suggests that GS might be acquired rather than inherited, but the pathogenesis remains elusive. It is postulated that a failure of the thymic selection processes may result from the disordered neoplastic thymic epithelium in GS [2]. The fact that GS has more severe clinical phenotype might be attributed to the coexistence of T cell dysfunction and absence of B cells [4].
National Cancer Institute data from the USA reported an incidence of 0.13 per 100 000 population for thymoma [5]. The association between thymoma and immunodeficiency has been less well defined. This rare disease entity needs standardized management guidelines, which are lacking, warranting prospective international, multi-center collaboration in data collection. Treatment should be personalized and modified on a case-specific basis.
Retrospective case series showed that GS has excellent long-term survival rates [6], with complete surgical resection being the key prognostic factor [7]. Notably, hypogammaglobulinemia, which constitutes about 10% of thymoma cases, is uncommonly corrected following thymus removal [8]. This does not necessarily translate into poor clinical outcome, as evidenced by the absence of worsening or new infection episodes in our patient after starting IVIG replacement. This is in parallel with a retrospective review which showed most patients (about 80%) had a significant reduction in the infection rates after IVIG treatment [9,10].
Studies have reported an increased susceptibility to bacterial, viral, and fungal infections, as well as autoimmunity, in patients with GS [2,3]. Opportunistic viral pathogens are reported to be the most common infectious culprit found in GS, in particular, CMV infection [4]. This might be explained by the fact that cytokines released by bone marrow stromal cells impair both thymic and B cell precursor growth and differentiation, and that thymic T cells exert a direct inhibitory effect on B cell immunoglobulin production [11]. CMV retinitis is more frequently reported in HIV patients, but sometimes it can also be found in the HIV-negative population, particularly in cases where there are factors contributing to immune dysregulation, for instance, GS [12]. Significant intraocular inflammation is not uncommon in CMV retinitis, in which the long-term visual outcome is often poor, especially in those with macular involvement [13], as in our patient. To the best of our knowledge, there is only 1 reported case of concomitant CMV retinitis and bronchiectasis associated with GS [14]. It was reported that the number of lymphocytes, which was normal prior to the onset of CMV disease, decreased during the active phase of disease, followed by an increase in the lymphocyte count later during the recovery stage [15]. This was seen in our patient, whose ALC dropped during the CMV disease and subsequently recovered after the resolution of infection.
Our patient developed severe neutropenic sepsis during the IV ganciclovir treatment. This was likely due to the bone marrow-suppressive effect of the systemic ganciclovir, which complicated further the immunosuppressive status of this patient. Ganciclovir is known to have hematological toxicity, which may be enhanced by CMV itself. CMV has a particular tropism for bone marrow cells, and it directly and indirectly damages these cells [16].
Conclusions
Our case highlights the challenge posed in managing a patient with immunodeficiency in association with thymoma. Clinicians should be aware that thymoma can precede the onset of immunodeficiency. Clinical suspicion should be heightened in at-risk patients who present with multiple bouts of infection, particularly in thymoma cases with adult-onset immune dysfunction. It is of paramount importance to follow up those patients with annual clinical reviews and immunodeficiency screening, which includes flow cytometric lymphocyte enumeration and immunoglobulin quantitation, as cases of progressive immune disorders have been reported.
Figures
References:
1.. Engels EA, Pfeiffer RM, Malignant thymoma in the United States: Demographic patterns in incidence and associations with subsequent malignancies: Int J Cancer, 2003; 105; 546-51
2.. Kelesidis T, Yang O, Good’s syndrome remains a mystery after 55 years: A systematic review of the scientific evidence: J Clin Immunol, 2010; 135(3); 347-63
3.. Malphettes M, Gerard L, Galicier L, Good syndrome: An adult-onset immunodeficiency remarkable for its high incidence of invasive infections and autoimmune complications: Clin Infect Dis, 2015; 61(2); e13-19
4.. Kelleher P, Misbah SA, Review: What is Good’s syndrome? Immunological abnormalities in patients with thymoma: J Clin Pathol, 2003; 56(1); 12-16
5.. Engels EA, Epidemiology of thymoma and associated malignancies: J Thorac Oncol, 2010; 5; S260-5
6.. Jansen A, Deuren M, Miller J, Prognosis of Good syndrome: Mortality and morbidity of thymoma associated immunodeficiency in perspective: Clin Immunol, 2016; 171; 12-17
7.. Zhao Y, Shi J, Fan L, Surgical treatment of thymoma: An 11-year experience with 761 patients: Eur J Cardiothorac Surg, 2016; 49; 1144
8.. Lee A, Chockalingam G, Good syndrome: Immunodeficiency associated with thymoma: Intern Med J, 2018; 48; 891-92
9.. Tarr PE, Sneller MC, Mechanic LJ, Infections in patients with immuno-deficiency with thymoma (Good syndrome). Report of 5 cases and review of the literature: Medicine, 2001; 80; 123-33
10.. Thongngarm T, Boonyasiri A, Pradubpongsa P, Features and outcomes of immunoglobulin therapy in patients with Good syndrome at Thailand’s largest tertiary referral hospital: Asian Pac J Allergy Immunol, 2019; 37(2); 109-15
11.. Oritani K, Medina KL, Tomiyama Y, Limitin: An interferon-like cytokine that preferentially influences B lymphocyte precursors: Nat Med, 2000; 6; 659-99
12.. Downes KM, Tarasewicz D, Weisberg LJ, Cunningham ET, Good syndrome and other causes of cytomegalovirus retinitis in HIV-negative patients – case report and comprehensive review of the literature: J Ophthalmic Inflamm Infect, 2016; 6(1); 3
13.. Iu LP, Fan MC, Lau JK, Long-term follow-up of cytomegalovirus retinitis in non-HIV immunocompromised patients: Clinical features and visual prognosis: Am J Ophthalmol, 2016; 165; 145-53
14.. Assi AC, Lightman S, Cytomeagalovirus retinitis in patients with Good syndrome: Arch Ophthalmol, 2002; 120(4); 510-12
15.. Castro SM, Sporleder H, Schroeder R, Lymphocyte subpopulations during cytomegalovirus disease in renal transplant recipients: Braz J Med Biol Res, 2003; 36(6); 795-805
16.. Holberg-Petersen M, Rollag H, Overli I, Direct growth suppression of myeloid bone marrow progenitor cells but not cord blood progenitors by human cytomegalovirus in vitro: Blood, 1996; 88(7); 2510-16
Figures
In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943042
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942578
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943801
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942966
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250