03 May 2021: Articles 
Bilateral Retinal Vasculitis as the First Presentation of Systemic Lupus Erythematosus
Unusual clinical course
Eaman Alhassan1ABEF*, Hannah K. Gendelman1ABEF, Marwa M. Sabha2ABEF, Melissa Hawkins-Holt3BE, Bernadette C. Siaton2EFDOI: 10.12659/AJCR.930650
Am J Case Rep 2021; 22:e930650
Abstract
BACKGROUND: Systemic lupus erythematosus (SLE) can involve any part of the eye. Keratoconjunctivitis sicca (dry eye) is the most common ocular manifestation, followed by scleritis, episcleritis, and retinitis. Retinal disease affects around 10% of patients with SLE. Mild retinopathy may be asymptomatic. However, severe cases can cause visual loss requiring urgent ophthalmic evaluation.
CASE REPORT: We present a case of bilateral retinal vasculitis as the presenting manifestation of SLE. A 14-year-old girl with a history of schizophrenia presented to the emergency department (ED) with generalized weakness. Four days before her presentation, she developed itching in her eyes and frontal headaches. In the ED, she reported blurry vision in her left eye only and diffuse arthralgia. The ophthalmic evaluation showed bilateral reduced visual acuity, worse in the left eye. Both eyes had diffuse hemorrhages, white retinal lesions, and blurred optic disc margins. She was diagnosed with panuveitis and retinal vasculitis. The patient was then found to have SLE, diagnosed by the presence of arthralgias, panuveitis, severe bilateral retinal vasculitis, positive ANA and anti-dsDNA, and normocytic anemia. The patient received intravenous methylprednisolone with subsequent oral prednisone upon discharge, hydroxychloroquine, and azathioprine. One year after her presentation, she had significant visual improvement and no other system involvement.
CONCLUSIONS: Retinal vasculitis, as the presenting symptom of SLE, has been overlooked in large studies. However, the number of case reports documenting this as a presenting symptom, often with minimal or no organ involvement, suggests that upon diagnosis, patients might benefit from a skilled ophthalmic evaluation.
Keywords: Lupus Erythematosus, Systemic, Retinal Vasculitis, Retinitis, Adolescent, Methylprednisolone, Scleritis, Vision Disorders
Background
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease with a strong predisposition in females of childbearing age. Worldwide, SLE is more prevalent in non-White populations. In the United States, it is more common in African Americans, who also have worse disease outcomes [1,2]. The clinical presentation varies widely among patients and can change throughout the disease course. SLE can affect different organs. The most common manifestations include fatigue, skin disease, arthralgia, renal, and neuropsychiatric symptoms.
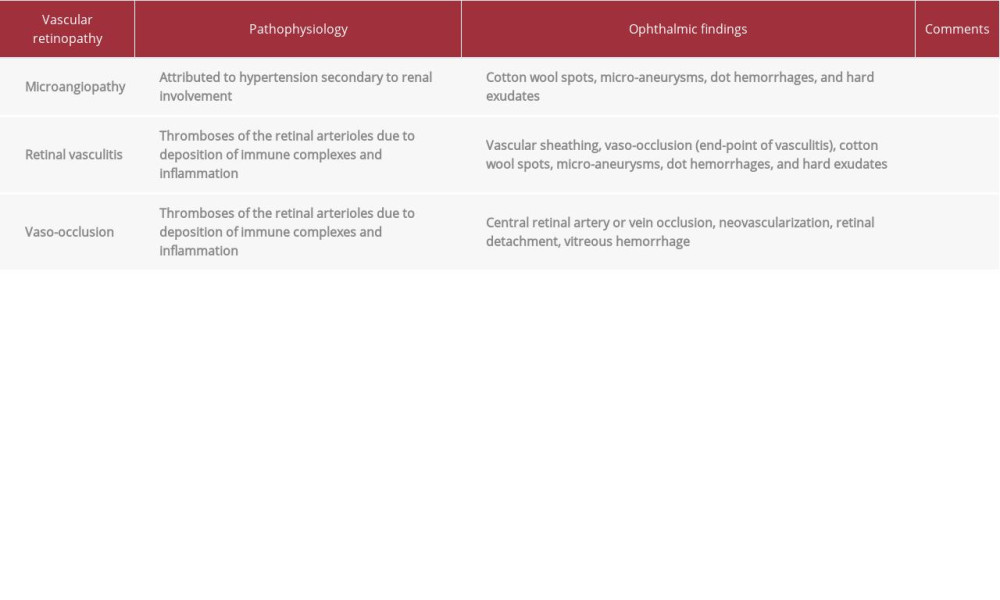
Systemic lupus erythematosus can also involve any part of the eye and visual pathway through inflammatory or thrombotic processes. Ocular manifestations were reported in about one-third of patients with SLE [3], and they can be useful indicators of disease activity [3,4]. Keratoconjunctivitis sicca (dry eye) is the most common ocular manifestation of SLE. Other common ocular manifestations include scleritis and episcleritis [5]. Mild retinopathy may be asymptomatic, but severe disease can cause loss of vision and requires urgent ophthalmic evaluation. The etiologies of lupus retinopathy include micro-angiopathy related to lupus renal disease and secondary hypertension, vaso-occlusion due to hypercoagulable state, or vasculitis (Table 1). We report the case of a 14-year-old girl presenting with bilateral retinal vasculitis as the first manifestation of SLE.
Case Report
A 14-year-old girl with a history of schizophrenia presented to the emergency department (ED) with generalized weakness. Four days before her presentation, she developed itching in her eyes and frontal headaches. She was taken to the urgent care clinic, diagnosed with allergic conjunctivitis, and prescribed antihistamine eye drops. One day later, she developed worsening weakness in her upper and lower extremities, causing difficulty ambulating. In the ED, she reported blurry vision in her left eye only. A review of systems was notable for fatigue, poor appetite, headaches, and arthralgias. Her vital signs were notable for a temperature of 39°C, blood pressure of 79/66 mmHg, and a heart rate of 110 beats/min. The physical examination was notable for bilateral conjunctival injection, non-reactive left pupil, 4/5 muscle strength in bilateral upper and lower extremities, and diffuse joint tenderness. The laboratory work-up was notable for hemoglobin of 10.4 g/dL (11.9–14.7), an erythrocyte sedimentation rate (ESR) of 121 mm/hr (0–20), C-reactive protein (CRP) of 3.9 mg/L (0–8), and creatine kinase (CK) of 51 U/L (26–192). Cytomegalovirus IgM (CMV IgM) was 39.8 AU/mL (0–29.9). Iron studies and aldolase were not obtained. Urinalysis was within normal limits. The ophthalmic evaluation showed reduced visual acuity in both eyes, more significant in the left. Both eyes had diffuse hemorrhages, white retinal lesions, and blurred optic disc margins. The patient was started on 1% atropine eye drops, prednisolone acetate eye drops, and intravenous (IV) ganciclovir for CMV retinitis. She also received an intravitreal injection of foscarnet in both eyes. After a few days, culture results from the aqueous humor did not show any detectable CMV, and ganciclovir was subsequently discontinued. A rheumato-logical work-up showed a positive antinuclear antibody (ANA) of >1: 2560 (<1: 40) in a homogenous pattern and anti-double stranded DNA (anti-dsDNA) of 1: 640 (<1: 10). Smith antibodies, SSA, SSB, and RNP, were normal. Complement levels (C3 and C4) were normal. Antiphospholipid syndrome (APS) antibodies were not obtained. The patient was diagnosed with SLE based on the presence of arthralgias, panuveitis, severe bilateral retinal vasculitis, positive ANA and anti-dsDNA, and normocytic anemia. The patient received intravenous methylprednisolone 60 mg daily for 5 days, followed by oral prednisone 60 mg daily. She was also started on azathioprine 50 mg daily and hydroxychloroquine 300 mg daily. She was also maintained on steroid eye drops and discharged home with close rheumatology and ophthalmology follow-up. Subsequently, hydroxychloroquine was stopped due to concerns of worsening ocular disease, and the azathioprine dose was increased to 100 mg daily. One year after her presentation, she reports significant improvement in her vision and overall good control of her SLE.
Discussion
Keratoconjunctivitis sicca is the most common ocular manifestation of SLE, followed by retinitis, scleritis, and episcleritis [6]. Retinal vasculitis is caused by thromboses of the retinal arterioles due to deposition of immune complexes and inflammation [7]. Our case represents an unusual presentation of retinal vasculitis as the presenting feature of SLE with no other organ involvement. Retinopathy is seen in 3–29% of patients with SLE [8]. Our patient presented with acute vision change from panuveitis and retinal vasculitis as her only manifestation of the disease, making this case unique. In the literature, this has been reported in a few cases: Purtscher-like retinopathy was described as the presenting symptom of a 15-year-old girl in India who was successfully treated with steroids and hydroxychloroquine [9]. Other cases of retinal vasculitis include a 13-year-old boy with photosensitive SLE rashes [10] and a 19-year-old girl with sudden vision loss whose vasculitis was felt to be entirely inflammatory with no vaso-occlusive contribution to the retinopathy [7]. As this review shows, retinal involvement is a known phenomenon associated with SLE. However, its etiology and extent are quite variable. Stafford-Brady et al found that retinopathy was correlated with active SLE in 88% of patients [11]. A small prospective study of patients with known SLE showed that of the 7 who developed retinopathy over 5 years, 6 were experiencing flares at the time of presentation [12]. Ushiyama et al found that higher Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) scores were associated with retinopathy [13], as was the presence of antiphospholipid antibodies [13]. It was also found that SLE patients with retinopathy had more proteinuria and higher serum creatinine levels, suggesting it is more common in patients with renal involvement [13]. However, several questions require further investigation. It is notable that the 3 cases noted above, who are similar in age and presentation to our case-patient, are not of African American descent. Reviews have tried to correlate disease activity and specific organ systems affected by race; however, many confounders have made this difficult [14]. In particular, there is variance in which, if any, ophthalmic findings are included in disease activity scoring systems. SLEDAI -2k includes “visual disturbance”, while the British Isles Assessment Group-2004 (BILAG-2004) specifies which part of the eye is involved and to what extent. The European Consensus Lupus Activity Measurement (ECLAM) does not include ocular manifestations. The American College of Rheumatology (ACR) classification criteria also do not include ocular involvement. Retrospective studies in the prevalence and progression of ocular disease are therefore hindered by the fact that patients with new SLE who lack visual symptoms do not undergo a detailed ophthalmic exam at the time of diagnosis [15,16]. Dammacco et al note that sicca is the only ocular symptom mentioned in several large multi-center studies, which is concerning for missed silent eye disease [15]. Tolba et al emphasized the importance of performing a fundus fluorescein angiography (FFA) assessment in SLE patients. FFA detected retinal disease even in patients with normal fundus examination results [17].
The treatment of retinal vasculitis is primarily related to treating the underlying cause, which in this case is SLE. Treatment consists of high doses of systemic glucocorticoids and adjunctive periocular or intraocular glucocorticoids, which our patient received and resulted in significant improvement in her vision.
Conclusions
SLE can involve any part of the eye and visual pathway, with keratoconjunctivitis sicca being the most common ocular manifestation. Other manifestations include scleritis, episcleritis, retinitis, uveitis, and optic neuritis. Retinal disease affects around 3–29% of patients with SLE. While large studies have overlooked retinopathy in SLE, the number of case reports documenting this as a presenting symptom, often with little other organ involvement, suggests that upon diagnosis, patients should have a skilled ophthalmic exam and that perhaps visual manifestations of disease should be included in the diagnostic criteria.
References:
1.. Bernatsky S, Boivin JF, Joseph L, Mortality in systemic lupus erythematosus: Arthritis Rheum, 2006; 54(8); 2550-57
2.. Pons-Estel GJ, Alarcón GS, Scofield L, Understanding the epidemiology and progression of systemic lupus erythematosus: Semin Arthritis Rheum, 2010; 39(4); 257-68
3.. Silpa-Archa S, Lee JJ, Stephen Foster C, Ocular manifestations in systemic lupus erythematosus: Br J Ophthalmol, 2016; 100(1); 135-41
4.. Arevalo JF, Lowder CY, Muci-Mendoza R, Ocular manifestations of systemic lupus erythematosus: Curr Opin Ophthalmol, 2002; 13(6); 404-10
5.. Sivaraj RR, Durrani OM, Denniston AK, Ocular manifestations of systemic lupus erythematosus: Rheumatology, 2007; 46(12); 1757-62
6.. Cunningham ET, Tabbara KF, Zierhut M, Systemic lupus erythematosus and the eye: Ocul Immunol Inflamm, 2018; 26(8); 1143-45
7.. Barkeh HJ, Muhaya M, Optic neuritis and retinal vasculitis as primary manifestations of systemic lupus erythematosus: Med J Malaysia, 2002; 57(4); 490-92
8.. Davies JB, Rao PK, Ocular manifestations of systemic lupus erythematosus: Curr Opin Ophthalmol, 2008; 19(6); 512-18
9.. Palkar AH, Hossain MD, Majumder PD, Purtscher-like retinopathy as presenting manifestation of systemic lupus erythromatosus following high-grade fever with myalgia and arthralgia: Indian J Ophthalmol, 2018; 66(9); 1317-19
10.. Bandyopadhyay SK, Moulick A, Dutta A, Retinal vasculitis – an initial presentation of systemic lupus erythematosus: J Indian Med Assoc, 2006; 104(9); 526-27
11.. , Lupus retinopathy – Stafford-Brady – 1988 – Arthritis’ Rheumatism– Wiley Online Library Accessed October 14, 2020. https://onlinelibrary-wiley-com.proxy-hs.researchport.umd.edu/doi/abs/10.1002/art.1780310904?sid=nlm%3Apubmed
12.. Klinkhoff AV, Beattie CW, Chalmers A, Retinopathy in systemic lupus erythematosus: Relationship to disease activity: Arthritis Rheum, 1986; 29(9); 1152-56
13.. Ushiyama O, Ushiyama K, Koarada S, Retinal disease in patients with systemic lupus erythematosus: Ann Rheum Dis, 2000; 59(9); 705-8
14.. Lewis MJ, Jawad AS, The effect of ethnicity and genetic ancestry on the epidemiology, clinical features and outcome of systemic lupus erythematosus: Rheumatology (Oxford), 2017; 56(sSuppl.1); i67-i77
15.. Dammacco R, Systemic lupus erythematosus and ocular involvement: An overview: Clin Exp Med, 2018; 18(2); 135-49
16.. Gao N, Li MT, Li YH, Retinal vasculopathy in patients with systemic lupus erythematosus: Lupus, 2017; 26(11); 1182-89
17.. Tolba DA, El-Fayoumi DMS, Abdelaziz MS, Nabih MH, Fluorescein angio-graphic findings in patients with active systemic lupus erythematosus: Ocul Immunol Inflamm, 2017; 25(6); 884-90
In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250