13 July 2021: Articles 
Congenital Dual Internal Hernias Causing Small Bowel Obstruction in a Man with no Prior Surgical History: A Report of a Very Rare Case
Challenging differential diagnosis, Management of emergency care, Rare disease
Shariful Islam12ABCDEFG*, Aneela N. Shah12ABCDEFG, Sarah Dial12ABEFG, Avidesh MahabirDOI: 10.12659/AJCR.932132
Am J Case Rep 2021; 22:e932132
Abstract
BACKGROUND: Internal hernias involve protrusion of the small bowel through a peritoneal or mesenteric space in the abdominal or pelvic cavity. Congenital internal small bowel hernias are rare and patients with them usually present with small bowel obstruction (SBO) at a young age, whereas in older patients, internal small bowel hernias usually are acquired secondary to previous surgery. The present report is of a rare case of SBO due to dual congenital internal small bowel hernias in a 51-year-old man with no history of abdominal surgery.
CASE REPORT: We report a case of dual congenital internal hernias of the small bowel in a patient who presented with symptoms and signs of SBO. He had no history of abdominal trauma, surgery, or comorbid conditions. His abdomen was mildly distended with minimal tenderness in the upper left quadrant but there was no guarding or rebound tenderness. Abdominal X-rays confirmed the SBO. A contrast-enhanced computed tomography scan of the patient’s abdomen revealed SBO with transition at 2 points, suggestive of a closed-loop obstruction. However, the exact cause of the SBO was confirmed at laparotomy, which revealed dual internal hernias (intramesosigmoid and paraduodenal). The hernias were managed individually and the patient had a successful outcome after surgery.
CONCLUSIONS: Although the present report is of a rare presentation of internal small bowel hernia, the case underscores that patients with this condition may present with SBO. Successful surgical management requires knowledge of the intra-abdominal peritoneal spaces and management of the hernia sac.
Keywords: Intestinal Obstruction, Laparoscopy, Laparotomy, case reports, Abdominal Pain, Hernia, Abdominal, Internal hernia, Intestine, Small
Background
Internal hernias are protrusions of abdominal viscus through the defects of the gastrointestinal mesentery or peritoneum-lined fossa [1]. They have unique pathology and are found in only 1% of the population, yet they account for almost 6% of all cases of small bowel obstruction (SBO) [2]. More importantly, mortality from a strangulated bowel can reach as high as 50% because this diagnosis easily can be overlooked. In a patient who has no history of surgery, congenital peritoneal defects allow the abdominal viscera to become easily entrapped [3–5]. Internal hernias, however, seem to be more common, with an increasing trend after procedures such as gastric bypass and liver transplantation [3,4].
Symptoms associated with internal herniation can be vague and early diagnosis is not always straightforward. Computed tomography (CT) is now considered the criterion standard for radiologic assessment of patients with suspicious symptoms or signs, especially for intestinal obstruction in a virgin abdomen [5]. Surgery is recommended for any patient diagnosed with an internal hernia and it is necessary when the condition is associated with acute intestinal obstruction. The optimal approach, however, is debatable. Several cases have been successfully managed with laparoscopy, although laparotomy may be preferable in the presence of significant bowel distension, necrosis, or a lack of laparoscopic skill or resources.
The present report is of a rare case of SBO due to dual congenital internal small bowel hernias in a 51-year-old man with no history of abdominal surgery, which was successfully managed with an open surgical repair. The clinical features, diagnosis, and options for management of internal hernias are discussed.
Case Report
A 51-year-old man was admitted because of a 3-day history of colicky abdominal pain with distension, constipation, and bilious vomiting. He had no history of abdominal trauma or surgery and no past medical conditions. He was a non-smoker and was able to perform all activities of daily living. During examination, the patient’s vital signs were within normal limits. His abdomen was distended, with tenderness in the upper left quadrant. There were no signs of peritonitis and no palpable masses or external hernias were identified. Bowel sounds were sluggish and digital rectal examination was normal. Results of blood tests were normal. On abdominal X-ray, however, dilated loops of small bowel with multiple air-fluid levels were visible (Figure 1).
Computed tomography (CT) of the abdomen and pelvis with i.v. contrast showed small bowel clustered in the upper left quadrant, dilated up to 4.4 cm in diameter. Two transition points were identified: one to the left of the duodenum (Figure 2) and another in the left iliac fossa (Figure 3), suggesting a closed-loop obstruction. The patient was adequately resuscitated and consented to surgery. We considered a laparoscopic approach, but our institution had restricted the use of emergent laparoscopy during the COVID-19 pandemic. This was because of the unavailability of timely preoperative COVID-19 testing, lack of a smoke evacuation system, and insufficient personal protective equipment. Therefore, the patient underwent an emergent laparotomy.
During the procedure, a segment of mid-ileum was found to be entrapped in a 3.5-cm defect on the lateral aspect of the sigmoid mesentery (Figure 4) and a similar segment of the mid-jejunum was also entrapped in the left paraduodenal fossa (Figure 5). Constriction was evident at both anatomical sites. The proximal and the intervening loop of small bowel were dilated and the SB distal to the sigmoid mesocolon hernia was collapsed. The entrapped bowel was easily reduced and there was no small bowel ischemia. No other pathology was identified.
The patient’s sigmoid mesocolon defect was repaired with interrupted absorbable sutures and his left paraduodenal defect was widened by opening its avascular boundary inferior-ly. His recovery after surgery was uneventful, with return of bowel function on day 2. He was discharged from the hospital on day 4. At 1-year follow-up, the patient was doing well, with no further symptoms.
Discussion
SBO due to dual internal hernias is rare in men with no surgical history; however, it should be considered in the differential when managing these patients.
Internal hernias can be broadly classified into acquired and congenital. Most classification systems distinguish congenital internal hernias based on their anatomic location. Meyers described them based on the location of the defect (Table 1) [3,6–9].
First described in by Moynihan in 1906, paraduodenal hernias have traditionally comprised the majority of internal hernias (53%) [1,10]. They occur when intestinal loops move into an abnormal fossa on either side of the duodenum [11]. Although they are thought to exist from birth, herniation (mostly of jejunal loops) occurs at age 40 to 60 years. Seventy-five percent of paraduodenal hernias are on the left side [3,10]. At the Landzert fossa, the mesenteries of the descending and trans-verse colon and small bowel converge. The inferior mesenteric vein and ascending branch of the left colic artery run along the lateral aspect of the fossa [3]. Few paraduodenal hernias become symptomatic. However, mortality reaches 20% to 50%, mainly because of missed diagnoses [1,11,12]. In our case, the patient’s left paraduodenal hernia was symptomatic; it was noted on CT scan and confirmed on laparotomy. The patient’s bowel was not compromised and he had a successful outcome.
Sigmoid mesocolon hernias represent less than 10% of internal hernias and are classified by Benson and Killen as intersigmoid, transmesosigmoid, or intramesosigmoid [13,14]. An intersigmoid hernia occurs when the small bowel passes through a recess between the sigmoid mesentery and the white line of Toldt. This recess is found in 65% to 75% of autopsy specimens and not all clinicians consider it to be a true aperture [3].
A transmesosigmoid hernia involves a typically small, oval-shaped defect that traverses completely through the sigmoid mesocolon with inferior mesenteric artery branches running along its edges. Herniated bowel lies posterior to the sigmoid colon with no associated sac [7,13,15]. The least common sub-type (intramesosigmoid) also involves a small, oval-shaped defect. However, only a single peritoneal leaf of the mesentery (usually the lateral) is involved. Thus, the herniated contents lie within the sigmoid mesentery. The risk of strangulation with an intersigmoid hernia is almost 14% [3,10,13–15]. Our patient was noted to have a 3.5-cm intramesosigmoid defect and there was no sign of bowel ischemia.
Internal hernias can remain asymptomatic or patients with them may present with abdominal pain and nausea after eating [3]. A characteristic feature of a paraduodenal hernia is postpran-dial abdominal pain that is relieved with postural changes. However, incarceration with intestinal obstruction represents a surgical emergency because a closed-loop obstruction occurs. As evidenced by the present case, diagnosis can be easily overlooked because of non-specific symptoms.
CT is considered the criterion standard for preoperative detection of an internal hernia. Adding i.v. contrast helps assess viability of the herniated contents and delineate the boundaries of the defect [10]. CT is easy to access, the imaging time is short, and it has high sensitivity and specificity (94% to 100% and 90% to 95%, respectively) [10,16]. Obstruction within an internal hernia is most often identified as a closed-loop picture with a distended, fluid-filled C- or U-shaped loop of intestine. Mesenteric vessels in the affected intestinal segment also may appear to be twisting or converging toward a central point [3,10]. CT features of left paraduodenal and sigmoid mesocolon hernias are described in Table 2 [1,10,14–16]. Our patient’s CT scan confirmed SBO with transition at 2 points, suggestive of closed-loop obstruction.
The aims of surgical treatment for all internal hernias are to reduce the contents, resect non-viable bowel, restore normal anatomy, and repair the defect [1,11,17]. The entrapped small intestine, as in the present case, often can be easily manually reduced from a left paraduodenal hernia. The concern with surgical repair, though, is maintaining the integrity of the nearby mesenteric vessels and avoiding compromise to the vascularity of the intestine. Surgical management of left paraduodenal hernias has been well described by Wakabayashi et al [18].
As documented in most case reports, a left paraduodenal hernia defect can be sutured closed. The mesocolon tissue around the inferior mesenteric vein (IMV) is tacked to the mesenteric base at the posterior abdominal wall. The fourth part of the duodenum can be tacked to the lateral edge of the defect to recreate a ligament of Treitz. There appear to be no differences between absorbable and non-absorbable sutures or between interrupted and continuous closure in terms of outcomes with the procedure [19].
Another option is to widen the defect by incising along an inferior avascular plane [11]. In some reports, the IMV was ligated to adequately achieve a large enough space to prevent future incarceration [11,17,19]. In the present case, the defect was widened because closure was thought to compromise the integrity of the mesenteric vessels. Interestingly, the need for mesh has not been well explored: In a few cases, successful use of mesh has been documented for large (>5 cm) or recurrent hernias [11,20–22].
The average defect in sigmoid mesocolon hernias is comparatively smaller, and when herniated bowel cannot be easily reduced by gentle traction, it can be widened, taking care to preserve the sigmoid vessels. However, closure of the defect to prevent a recurrence is recommended [14]. In contrast, in 2014, Yang et al stated that an intramesosigmoid defect does not require closure, and instead it can be widened by dissecting the lateral peritoneal attachment of the sigmoid colon [21]. In the present case, the intramesosigmoid defect was closed with interrupted absorbable sutures.
Whether laparotomy or laparoscopy is the superior approach is still debatable because published evidence is based only on case reports and series. For elective cases, laparoscopy may be preferrable. It can be used to confirm the diagnosis if that was not established before surgery [11]. Watanabe et al documented successful elective treatment of an intersigmoid hernia via a single-incision laparoscopic approach [22]. However, in an emergency, management of sigmoid mesocolon hernias depends on the patient’s hemodynamic status, underlying conditions of the small bowel, and the availability of a skilled laparoscopic surgeon. Laparotomy is still the method of choice for acute cases of incarceration with bowel obstruction, strangulation, and ischemia.
Despite technical challenges, laparoscopy is now frequently used in the management of SBO, with a conversion rate of almost 24%, although bowel resection was performed in 12.6% [11,14,16]. However, in the hands of a skilled laparoscopic surgeon, it is possible to successfully manage some of these cases, even in the presence of gangrenous small bowel. Islam et al reported the world’s first case of laparoscopic management of SBO in a patient with gangrenous bowel, with minimal morbidity [23].
The occurrence of 2 internal hernias in the same patient appears to be unique. The application of surgical repair principles was successful and the inclusion of the present case in the surgical literature may add new information about the incidence of internal hernias.
Conclusions
Although the present report is of a rare presentation of internal small bowel hernias, it underscores that patients with the condition may present with SBO. Successful surgical repair requires knowledge of the intra-abdominal peritoneal spaces and management of the hernia sac.
Figures
References:
1.. Martin LC, Merkle EM, Thompson WM, Review of internal hernias: Radiographic and clinical findings: Am J Roenthgenol, 2006; 186; 703-17
2.. Ghiassi S, Nguyen SQ, Divino CM, Internal hernias: Clinical findings, management, and outcomes in 49 non-bariatric cases: J Gastrointest Surg, 2007; 11; 291-95
3.. Lanzetta MM, Masserelli A, Addeo G, Internal hernias: A difficult diagnostic challenge. Review of CT signs and clinical findings: Acta Biomed, 2019; 90(5); 20-37
4.. Akyildiz H, Artis T, Sozuer E, Internal hernia: Complex diagnostic and therapeutic problem: Int J Surg, 2009; 7; 334-37
5.. Dou L, Yang H, Wang C, Adhesive and non-adhesive internal hernia: Clinical relevance and multi-detector CT images: Sci Rep, 2019; 9(1); 12847
6.. Reddy U, Dev B, Santosham R, Internal hernias: Surgeons dilemma – unravelled by imaging: Indian J Surg, 2014; 76(4); 323-28
7.. Agarwal A, Ray U, Hossain M, Congenital intra-mesosigmoid hernia: A case report of a rare sigmoid mesocolon hernia: Indian J Surg, 2011; 73(6); 450-52
8.. Kulendran K, Keogh C, Chiam HC, Laparoscopic repair of a left para duodenal hernia: ANZ J Surg, 2017; 89(4); E172-73
9.. Hirashima K, Date K, Fujita K, Strangulation of the small intestine caused by an intra-mesosigmoid hernia: A case report: Surg Case Rep, 2017; 3; 129
10.. Karcz KW, Zhou C, Daoud M, Modification of internal hernia classification system after laparoscopic Roux-en-Y bariatric surgery: Videosurg Miniinv, 2015; 10(2); 197-204
11.. Kulkarni GV, Salaonkar HP, Sharma PC, Laparoscopic repair of left para duodenal hernia: Report of two cases and review of the literature: Asian J Endosc Surg, 2016; 9; 157-60
12.. Junttila A, Virtanen J, Mrena J, Laparoscopic treatment of small bowel strangulation caused by an intramesosigmoid hernia and review of literature: BMJ Case Rep, 2020; 13; e233627
13.. Nagano H, Goi T, Taguchi S, Diagnosis of incarcerated intra-mesosigmoid hernia aided by multi-planar reconstruction images of multi-detector computed tomography: A case report: Surg Case Rep, 2018; 4(1); 128
14.. Jimmy J, Wani SV, Shetty VV, Laparoscopic management of small bowel obstruction caused by a sigmoid mesocolic hernia: J Min Access Surg, 2011; 7(4); 236-38
15.. Jeong GA, Cho GS, Kim HC, Laparoscopic repair of para duodenal hernia comparison with conventional open repair: Surg Laparosc Endosc Percutan Tech, 2008; 18(6); 611-15
16.. Sleiman Y, El-Kheir A, El-Khoury M, Small bowel obstruction secondary to left para duodenal hernia: A case report and literature review: International J Surg Case Rep, 2018; 53; 29-31
17.. Poh BR, Sundaramurthy SR, Mirbagheri N, Left para duodenal hernia causing small bowel obstruction: J Gastrointest Surg, 2014; 18; 1377-78
18.. Wakabayashi M, Kono S, Takahashi T, Laparoscopic repair of acute small bowel obstruction due to left para duodenal hernia: A case report: International Journal of Surgery Case Reports, 2018; 51; 194-99
19.. Sakamoto T, Lefor A, Laparoscopic reduction and repair of a left para duodenal hernia: BMJ Case Rep, 2019; 12; e232098
20.. Xu H, Nie N, Kong F, Large left para duodenal hernia with intestinal ischemia: A case report and literature review: J Int Med Res, 2020; 48(9); 300060520955040
21.. Yang C, Kim D, Small bowel obstruction caused by sigmoid mesocolic hernia: J Surg Case Rep; 2014(5); rju036
22.. Watanabe T, Wada H, Sato M, Single-incision laparoscopic surgery for intersigmoid hernia: Case Rep Surg, 2014; 2014; 589649
23.. Islam S, Payne O, Bheem V, Laparoscopic resection of gangrenous small bowel with acute small bowel obstruction – World’s first reported case: Innovative Journal of Medical and Health Science, 2019; 9(3); 354-59
Figures
Tables
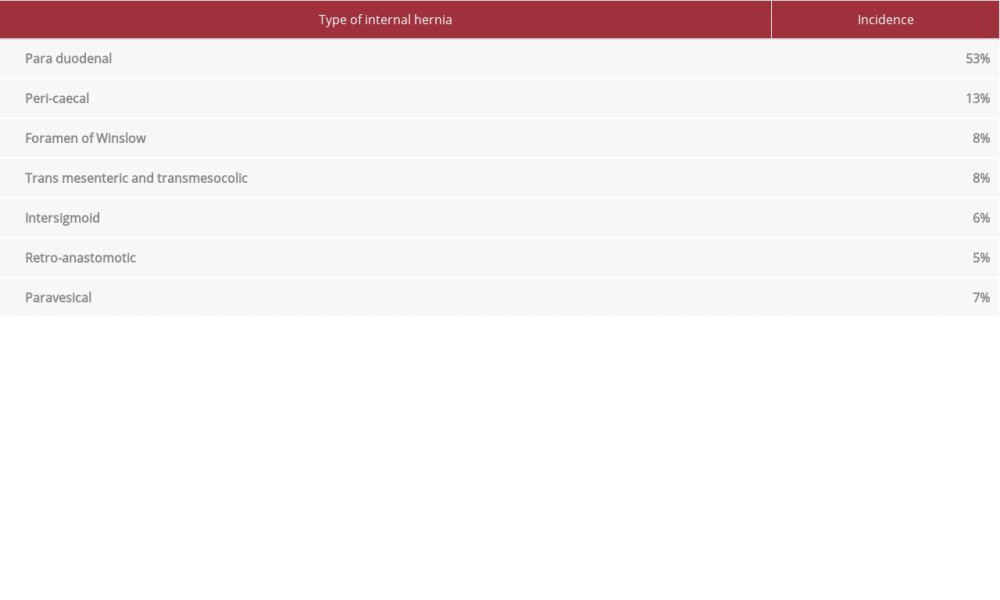 Table 1.. Meyer’s classification of internal hernias.
Table 1.. Meyer’s classification of internal hernias.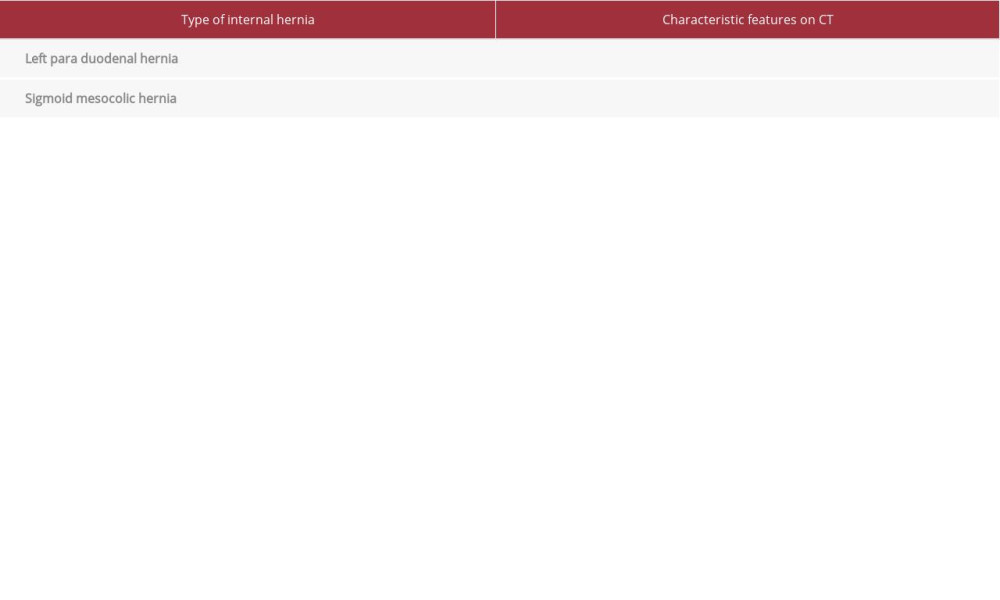 Table 2.. A computed tomography scan shows features of the left paraduodenal and sigmoid mesocolon hernias.
Table 2.. A computed tomography scan shows features of the left paraduodenal and sigmoid mesocolon hernias.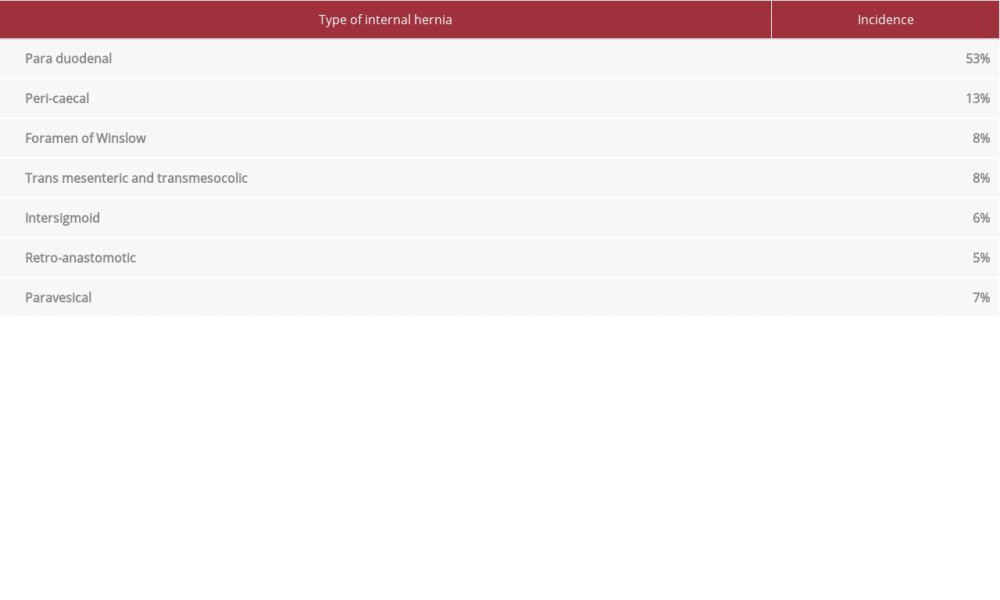 Table 1.. Meyer’s classification of internal hernias.
Table 1.. Meyer’s classification of internal hernias.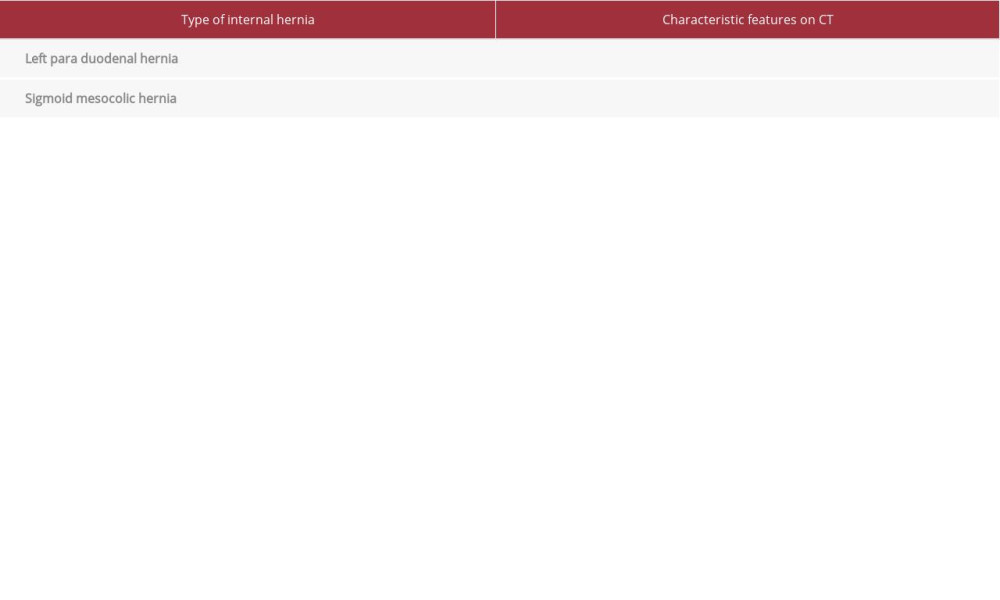 Table 2.. A computed tomography scan shows features of the left paraduodenal and sigmoid mesocolon hernias.
Table 2.. A computed tomography scan shows features of the left paraduodenal and sigmoid mesocolon hernias. In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








