21 July 2020: Clinical Research
Ureteroscopic Diagnosis and Povidone Iodine Treatment for Chronic Unilateral Hematuria Caused by Benign Lesions
Zhenghui Hu1E, Yan Zhang1B, Jiaxin Liu1C, Hongshen Wu1D, Feifan Wang1F, Xiaodong Jin1A*DOI: 10.12659/MSM.923552
Med Sci Monit 2020; 26:e923552
Abstract
BACKGROUND: The management of chronic unilateral hematuria (CUH) caused by benign lesions is a therapeutic challenge to many urologists. The aims of this study were to evaluate the efficacy and safety of povidone iodine sclerotherapy for CUH.
MATERIAL AND METHODS: We identified 20 patients who underwent povidone iodine sclerotherapy to treat CUH between September 2013 and August 2017. Radiologic and hematologic tests were normal, no definite cause of hematuria was revealed, and the malignant lesions were excluded. Cystoscopy and ureteroscopy indicated the lesions were located in the renal pelvis. The goal of successful treatment was no recurrence of hematuria during follow-up.
RESULTS: The present study analyzed 20 patients (9 females and 11 males), 24–73 years old (mean age 44.6) with mean follow-up of 23.8 (range 13–60) months. Endoscopic findings included discrete lesions, diffuse lesions, and no obvious lesion. Discrete lesions were identified as hemangioma (4/20, 20%), minute venous rupture (12/20, 60%), and varix (1/20, 5%). Diffuse lesions were founded via ureteroscopy in 2 (2/20, 10%) patients. In the remaining 1 (1/20, 5%) patient, no obvious lesion was found. All patients with CUH were treated with 0.5% povidone iodine for pelvicalyceal system instillation, which was given at 12-h intervals for 3 days. Only 1 patient experienced recurrent gross hematuria, after 24 months postoperatively. The overall success rate, defined as resolution of gross hematuria after povidone iodine sclerotherapy, was 95%. No complications were recorded.
CONCLUSIONS: The present study indicates that povidone iodine sclerotherapy could be an effective, safe, and minimally invasive treatment for chronic unilateral hematuria caused by benign lesions.
Keywords: Hematuria, Povidone-Iodine, Sclerotherapy, Ureteroscopy, Chronic Disease, Kidney Pelvis
Background
Chronic unilateral hematuria (CUH), defined as idiopathic renal hematuria, is characterized by continuous or intermittent gross hematuria originating from the upper urinary tract. Mostly, CUH cannot be diagnosed by standard radiology and hematology [1,2]. Sometimes it cannot easily be differentiated from life-threatening hemorrhage or malignant tumors. Even with further workup, the diagnosis of CUH may remain unidentified. Historically, nephrectomy was performed in some patients for possible malignancy or hemostasis. Use of endoscopic devices and techniques for diagnosing and treating CUH can avoid unnecessary nephrectomy, [3–5]. Some benign lesions were treated with endoscopic electrofulguration or laser ablation, but the effect of those treatments varied greatly among studies. Of those individuals whose lesions were not obvious, the cure rate and relapse rate were not satisfactory [6].
Recently, novel therapeutic options for CUH have been explored in animals [7,8]. As opposed to silver nitrate sclerotherapy, povidone iodine sclerotherapy might be an effective treatment for CUH in dogs. According to the literature, povidone iodine is a safe and effective sclerosing agent in the management of chyluria. However, whether povidone iodine sclerotherapy could be an option for treatment of CUH in humans is still under investigation.
Material and Methods
From September 2013 to August 2017, 20 patients with CUH were retrospectively enrolled in this study. All patients had normal results of urine cytology and hematologic tests, including blood coagulation time test and complete blood count. A phase-contrast microscopic examination of urinary erythrocytes also excluded glomerular hematuria. Radiological examinations, including renal ultrasonography and CT urogram (CTU), could not find any upper-tract pathological change, and cystoscopic examination showed that the hematuria originated from the unilateral upper urinary tract in all patients. No evidence of malignancy was found. After unilateral hematuria of all patients was confirmed by cystoscopy, we performed diagnostic ureteroscopy.
Rigid ureteroscopy and a flexible ureteroscopy were performed to evaluate the entire ipsilateral upper urinary tract. Under general anesthesia, patients were placed in dorsal lithotomy position. A 6.9-Fr rigid ureteroscope was inserted into the ureteral orifice of the affected side with a guide wire under direct vision. Once the rigid ureteroscope reached the renal pelvis, it was removed and a flexible ureteroscope was passed over the guide wire into the ureter. The proximal ureter and the renal pelvis were then carefully inspected.
Since bleeding from trauma can obscure the lesions in the collecting system, gentle irrigation was very important in the whole the procedure. Irrigation pressure throughout the procedure was maintained at 40 mmHg. If the source of bleeding was not clear, the irrigation flow was turned off and ureteroscopy was performed without irrigation so that the bleeding site could be identified.
Systemic evaluation of the upper ureter, renal pelvis, and upper-, middle-, and lower-pole calices was performed by flexible ureteroscopy. CUH can be divided into 3 types: no obvious lesion, discrete lesions, and diffuse lesions. When a suspected site was identified, a guide wire was cautiously placed into the renal pelvis. Then, the flexible ureteroscope was removed. A 6.0-Fr single-J stent was placed into the renal pelvis. Ten milliliters of sclerosant solution was prepared by mixing 2 ml of 5% povidone iodine and 18 ml of distilled water. The sclerosant solution was gently instilled into the pelvicalyceal system and maintained there for 5 min. Sclerosant solution was given at 12-h intervals for 3 days through the single-J stent, with the distal part of the stent clamped for 5 min after each instillation.
Follow-up included urinalysis at 1, 3, 6, and 12 months, and then annually postoperatively. Urine cytology and renal ultrasonic examination were performed every 3 months postoperatively. All patients completed a minimum follow-up of 1 year.
Results
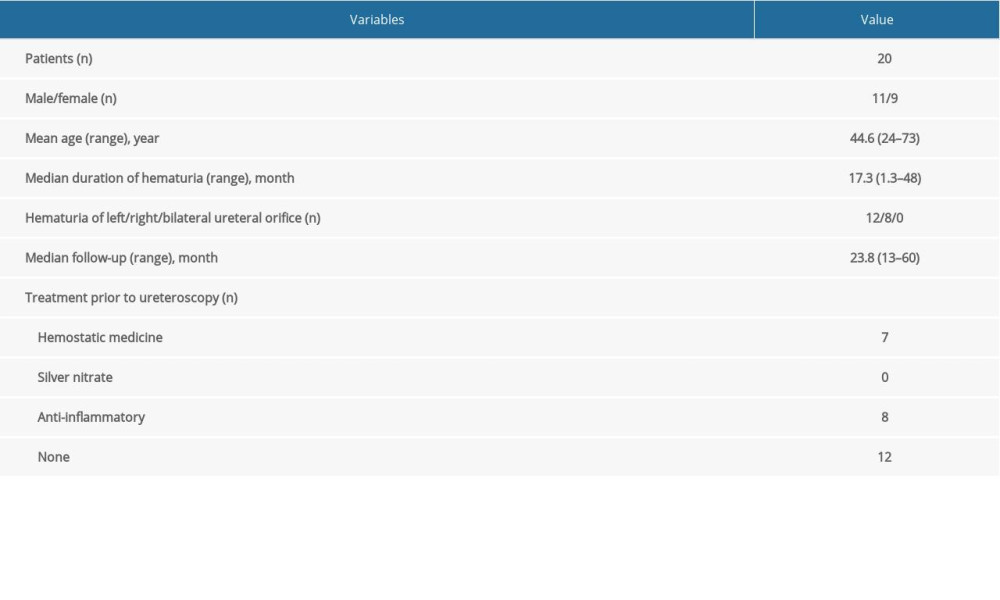
Twenty patients were identified for CUH, with a median age of 44.6 (range 24–73) years, including 11 males and 9 females (Table 1). Cystoscopy confirmed 12 (60%) patients had bleeding in the left ureteral orifice, 8 (40%) in the right side, and zero (0%) in both sides. Intermittent or continuous gross hematuria had occurred prior to ureteroscopy for 17.3 (range 1.3–48) months. Median follow-up was 23.8 (range 13–60) months. Seven patients had received hemostatic medication (carbazochrome sodium sulfonate, aminocaproic acid, or tranexamic acid) prior to ureteroscopy. Eight patients had received anti-inflammatory medication and 12 patients had never be treated. None of these previous treatments before ureteroscopic evaluation appeared to improve the symptoms of gross hematuria.
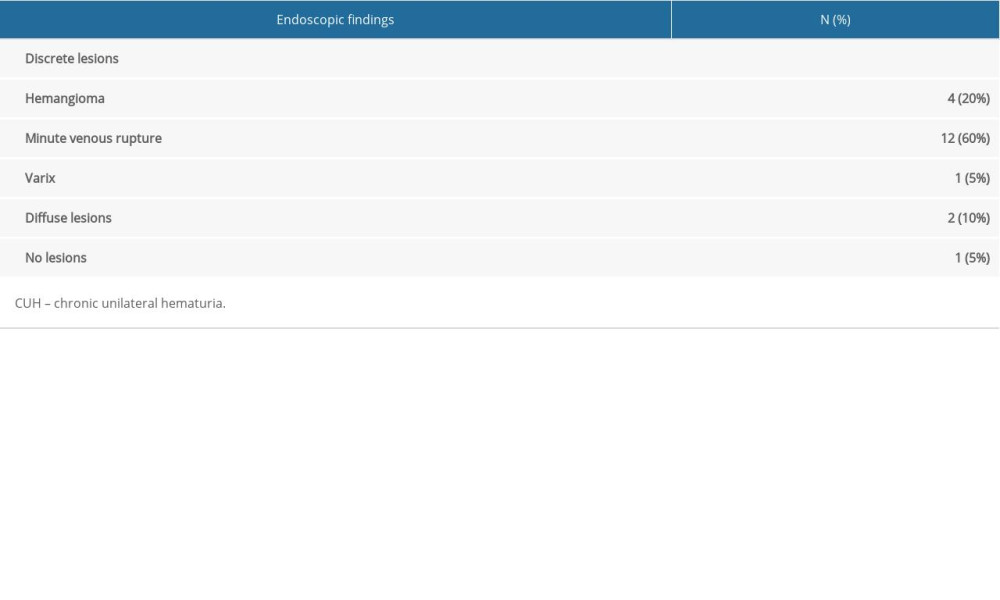
Complete visualization of the entire collecting system was performed ureteroscopically. Based on the examination, CUH can be divided into 3 types: discrete lesions, diffuse lesions, and no obvious lesion (Table 2). Discrete lesions included hemangioma (4/20, 20%), minute venous rupture (12/20, 60%), and varix (1/20, 5%). Diffuse lesions were found in 2 (10%) patients. In the remaining 1 (5%) patient, no obvious lesion was detected. Hemangiomas were usually in the papillary tips, which range in size from red spots to larger vascular-appearing lesions [9]. The size of the lesions was 2–3 mm in diameter. Minute venous rupture appeared as small lesions caused by the fragile vasculature of the renal papilla or fornix. In patients with typical endoscopic manifestation of a minute venous rapture in our study, a stream of blood from the tip of the renal papilla or fornix was identified. Peripapillary varices appeared as a tortuous vein over the papilla [10]. Two patients with diffuse lesions showed extensive congestion and edema of mucosa or multiple erosion of mucous membranes in the renal pelvis and calyces.
Patients with CUH were treated with 0.5% povidone iodine for pelvicalyceal system instillation. All patients were satisfied after the treatment. Only 1 patient experienced recurrent gross hematuria after 24 months. The overall cure rate, defined as resolution of gross hematuria after endoscopic treatment, was 95%. The longest follow-up time was 60 months. Urinalysis was normal at 1 month postoperatively. Urine cytology and renal ultrasonography were normal during follow-up. Furthermore, there was no complications associated with the ureteroscopic procedure and povidone iodine instillation.
Discussion
Historically, intravenous urography, renal ultrasonography, renal angiography, urine cytology, and abdominal computerized tomography are often used for detection of CUH, but the diagnosis is still often missed. Continuous or intermittent gross hematuria from a unknown source can lead to severe anemia and can be associated with significant renal colic due to blood clots [11]. Development of endoscopic technology has allowed less invasive and more accurate diagnosis and treatment for CUH when the malignant lesions were excluded [12,13]. A completed visualization of the collecting system and ureter is inspected to arrive at the final diagnosis of CUH by the ureteroscopic evaluation. In 1981, Gittes et al. first applied the technique of nephroscopy in patients with CUH; after nephroscopic examination, 12 patients underwent partial nephrectomy and 1 patient received nephrectomy [14]. Rigid and flexible endoscopy of the upper urinary tract has been available to urologists for the last 20 years. The indications for this procedure have increased, especially for detecting unknown hematuria.
In our series, minute venous rupture was the most common endoscopic finding, but its cause is still unknown. Lopatkin et al. reported that most renal hemorrhages appear as a result of the rupture of a thin-walled septum separating the veins from the collecting system, which may occur under high renal venous pressure or high intrapelvic pressure [15]. Kumon et al. reported that the rupture of a thin-walled vein found endoscopically appear as a minute venous rupture, although the cause of renal venous or renal pelvis high pressure is unclear [16]. To identify such a small minute venous rupture and have fewer unidentified lesions, we tried our best to ensure gentle irrigation for an excellent visual field.
In the past, nephrectomy and heminephrectomy were performed in some patients [17], but if the lesions are benign, removing the kidney is unacceptable in the current medical era. Moreover, the hematuria could be bilateral. With the development of a more comprehensive understanding of hematuria, it is now known that lesions mainly occur in the renal pelvis and calyces, not the kidney itself, so partial or total nephrectomy should be avoided to protect kidney function. Other traditional treatments include bed-rest, hemostasis, and irrigation of renal pelvis with silver nitrate. Silver nitrate, a chemical cauterizing and coagulating agent, has been used with renal pelvis irrigation to treat CUH [18]. However, silver nitrate irrigation in the renal pelvis is closely associated with symptoms of flank pain, nausea, vomiting, ureteral strictures, interstitial nephritis, pyonephrosis, and sepsis [19]. Due to this series of adverse events, the use of silver nitrate irrigation therapy is gradually decreasing. Recently, diathermy fulguration and laser treatment have been used clinically for patients with CUH. Diathermy fulguration is applied in more than 80% of all reported endoscopic treatments. Although diathermy fulguration is inexpensive, safe, and widely available, the efficacy is unclear. Many investigators also reported that ureteroscopic laser treatment is a useful method for CUH [20]. However, the laser rigidity is greater, which may prevent full deflection. Moreover, laser treatment is more suitable for limited and definite lesions in the renal pelvis and calyces. It is not suitable for the treatment of the diffuse lesions with extensive congestion and erosive mucous membranes.
Sclerotherapy treatment is more commonly used for chyluria and affects the extensive lymphatic communications in the renal pelvis [21]. Many studies reported that the cure rate of sclerotherapy with povidone iodine in the therapy of chyluria was 90% [22]. Berent and Adelman reported that povidone iodine sclerotherapy was safe and effective for treatment of CUH in dogs [7,8], but no clinical studies on povidone iodine sclerotherapy for CUH in humans were reported. We found that 0.5% povidone iodine sclerotherapy is an effective, safe, and minimally invasive way to treat CUH, and its use avoids nephrectomy. All of our patients tolerated the procedure of irrigation with povidone iodine into the renal pelvis. The gross hematuria of all patients resolved after 0.5% povidone iodine irrigation of the renal pelvis, which was given at 12-hintervals for 3 days. One patient with diffuse lesions experienced recurrent gross hematuria at 24 months postoperatively. No complications were found during follow-up.
Povidone iodine is a granulating and corrosive agent. The possible mechanism of treatment for hematuria is oxidizing potential that plays a role in the oxidation of local tissues and the heating effect that directly reduces bleeding. Povidone iodine can prevent urinary tract infection after irrigation. Additionally, the quality of povidone iodine can be controlled and it is readily available.
There are a few limitations of this study. First, the sample size was small. Second, the follow-up period was not long enough to assess long-term safety and effectiveness of the treatment. Well-designed, multiple-center, randomized controlled studies are needed to verify our findings in the future.
Conclusions
In conclusion, our findings suggest that povidone iodine sclerotherapy is an effective, safe, and minimally invasive treatment for CUH caused by benign lesions.
References
1. Lano MD, Wagoner RD, Leary FJ, Unilateral essential hematuria: Mayo Clin Proc, 1979; 54; 88-90
2. Dooley RE, Pietrow PK, Ureteroscopy for benign hematuria: Urol Clin North Am, 2004; 31; 137-43
3. Tawfiek ER, Bagley DH, Ureteroscopic evaluation and treatment of chronic unilateral hematuria: J Urol, 1998; 160; 700-2
4. Bagley DH, Removal of upper urinary tract calculi with flexible ureteropyeloscopy: Urology, 1990; 35; 412-16
5. Mugiya S, Ozono S, Nagata M, Ureteroscopic evaluation and laser treatment of chronic unilateral hematuria: J Urol, 2007; 178; 517-20
6. Rowbotham C, Anson KM, Benign lateralizing haematuria: The impact of upper tract endoscopy: BJU Int, 2001; 88; 841-49
7. Adelman LB, Bartges J, Whittemore JC, Povidone iodine sclerotherapy for treatment of idiopathic renal hematuria in two dogs: J Am Vet Med Assoc, 2017; 250; 205-10
8. Berent AC, Weisse CW, Branter E, Endoscopic-guided sclerotherapy for renal-sparing treatment of idiopathic renal hematuria in dogs: 6 cases (2010–2012): J Am Vet Med Assoc, 2013; 242; 1556-63
9. Hagen A, Renal angioma: Four cases of angioma of the renal pelvis: Acta Chir Scand, 1963; 126; 657-67
10. Takazawa R, Kitayama S, Tsujii T, Digital ureteroscopic visualization of lesions responsible for chronic unilateral hematuria, so-called idiopathic renal bleeding: Int J Urol, 2014; 21; 227-28
11. Patterson DE, Segura JW, Benson RC, Endoscopic evaluation and treatment of patients with idiopathic gross hematuria: J Urol, 1984; 132; 1199-200
12. Tanimoto R, Kumon H, Bagley DH, Development of endoscopic diagnosis and treatment for chronic unilateral hematuria: 35 years experience: J Endourol, 2017; 31; S76-80
13. Araki M, Uehara S, Sasaki K, Ureteroscopic management of chronic unilateral hematuria: A single-center experience over 22 years: PLoS One, 2012; 7; e36729
14. Gittes RF, Varady S, Nephroscopy in chronic unilateral hematuria: J Urol, 1981; 126; 297-300
15. Lopatkin NA, Morozov AV, Lopatkina LN, Essential renal haemorrhages: Eur Urol, 1978; 4; 115-19
16. Kumon H, Tsugawa M, Matsumura Y, Ohmori H, Endoscopic diagnosis and treatment of chronic unilateral hematuria of uncertain etiology: J Urol, 1990; 143; 554-58
17. Costa Neto TF, Renteria JM, Di Biase Filho G, Renal hemangioma: Int Braz J Urol, 2004; 30; 216-18
18. Diamond DA, Jeffs RD, Marshall FF, Control of prolonged, benign, renal hematuria by silver nitrate instillation: Urology, 1981; 18; 337-41
19. Dhabalia JV, Pujari NR, Kumar V, Silver nitrate sclerotherapy for chyluria: Evaluation for the optimal instillation regime: Urol Int, 2010; 85; 56-59
20. Brito AH, Mazzucchi E, Vicentini FC, Management of chronic unilateral hematuria by ureterorenoscopy: J Endourol, 2009; 23; 1273-76
21. Goel S, Mandhani A, Srivastava A, Is povidone iodine an alternative to silver nitrate for renal pelvic instillation sclerotherapy in chyluria?: BJU Int, 2004; 94; 1082-85
22. Sharma G, Chitale V, Karva R, Fluoroscopy guided instillation therapy in chyluria using combination of povidone iodine with contrast agent. Is a single instillation sufficient?: Int Braz J Urol, 2008; 34; 270-75 discussion 275–76
In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952