03 September 2020: Clinical Research
Relation Between Neck Pain and Modic Changes in Cervical Spondylotic Myelopathy
Yadong Sun1ABCE, Changzhi Yan2F, Yong Shen3BCD, Zhanyong Wu1AC*DOI: 10.12659/MSM.923908
Med Sci Monit 2020; 26:e923908
Abstract
BACKGROUND: Modic changes on magnetic resonance imaging (MRI) represent lesions in the bone marrow of the vertebral body that may be associated with pain. This study investigated the relationship between neck pain and cervical Modic changes, and risk factors for neck pain (NP).
MATERIAL AND METHODS: This study included 168 patients diagnosed with cervical spondylotic myelopathy between February 2013 and April 2017. Basic patient information about demographic and lifestyle variables was obtained from medical records. Radiographic images provided cervical alignment (C2–C7 Cobb), T1 slope and C7 slope. All patients underwent MRI to evaluate the presence of Modic changes. Univariate analyses identified the variables as potential factors. Variables with a p<0.10 were included in the multivariate logistic regression analysis models. P-values <0.05 were statistically significant.
RESULTS: Only 93 patients (55.4%) had NP. Modic changes in patients with NP were significantly higher than those without Modic changes (p=0.002). Eighty-five patients had Modic changes types I, II, III; 41 (48.2%), 29 (34.1%), 15 (17.6%), respectively. The distribution of these Modic changes varied with NP (p<0.001). Type I Modic changes were seen with NP more frequently than other types of Modic changes. Univariate and multivariate analyses showed that age (odds ratio [OR], 1.09; 95% confidence interval [CI], 1.02–1.16) and Modic changes (OR 1.25; 95% CI, 0.09–1.46) were significant independent factors for NP.
CONCLUSIONS: In cervical spondylosis, age and Modic changes were associated with NP. Modic change type I is more likely to occur with NP.
Keywords: Neck Pain, radiculopathy, Risk Factors, Magnetic Resonance Imaging, spondylosis
Background
Neck pain (NP) is a common symptom with a probability of 0.40% to 41.5% [1]. In the US, more than 40% adults suffer from chronic NP [2]. These adults endure the pain for an average of 10 years [3]. As NP is expensive to cure, it is becoming the fourth burden on people’s lives [4]. Cervical Modic changes are a degenerative phenomenon, seen as signal changes of vertebral endplates and subchondral bone on magnetic resonance imaging (MRI). Clinically, we found that NP in patients was often accompanied by cervical Modic changes. We suspect a connection between Modic changes and NP. In recent years, there has been considerable literature on the treatment of NP [5]. Some researchers studied the correlation between NP and high-density lipoprotein (HDL), low-density lipoprotein (LDL), and physical workload. The relationship between cervical sagittal range of motion (ROM) and the severity of NP has also been demonstrated [7]. However, there is little literature that demonstrates the relationship between Modic changes (MCs) and NP. It is important to recognize the risk factors for developing NP as this may be the guide to its prevention.
Material and Methods
PATIENT POPULATION:
This was a retrospective single-center study of 168 patients diagnosed with cervical spondylotic myelopathy between February 2013 and April 2017. They were divided into two groups based on the presence or absence of neck pain; NP (+), NP (−), respectively. Inclusion criteria were adults aged between 30 and 70 years; adults diagnosed with cervical spondylotic myelopathy for more than 1 month in an outpatient or ward setting. Exclusion criteria were trauma, infectious diseases, tumors, cervical spinal surgery, congenital malformation, and scoliosis. This study was approved by the Orthopedics Hospital of Xingtai City Ethics Committee. As the data were collected and analyzed anonymously in this single-center study, the Ethics Committee waived informed consent.
PARAMETER EVALUATION:
Data were collected to predict risk factors and divided into four categories, including demographic data, lifestyle variables, radiographic images and MRI images. Medical records contained demographic data and lifestyle variables such as age, gender, weight, height, body mass index (BMI), smoking and alcohol history. Radiographic images included C2–C7 Cobb, T1 slope and C7 slope. MRI images included three types of Modic changes. These definitions were measured in standing lateral radiographs (Figure 1). The terms used are defined as: C2–C7 Cobb is the angle between the inferior endplates of C2 and C7; T1 slope is the angle formed by the horizontal line and the superior endplate of T1; C7 slope is the angle formed by the horizontal line and the superior endplate of C7.
All the radiographs were performed by two experienced radiologic technologists. The reports were made by two investigators. In case of a disagreement, the final decision was made by a third image investigator.
STATISTICAL ANALYSIS:
IBM SPSS Statistics 21 (SPSS Inc., Chicago, IL, USA) was used for data analysis. Continuous variables were shown as mean±standard deviation, and categorical variables were presented as frequencies and percentages, analyzed by the Chi-square test or Kruskal-Wallis test.
Results
In total, 168 participants (79 males and 89 females) were included in this study. The average age was 51.1±12.4 years. Of these, 93 patients (55.4%) had NP, and the other 75 (44.6%) had no NP. All patient details, demographic data and clinical characteristics are shown in Table 1. The average age of patients with NP was significantly higher than those without NP (58.1±10.1 years
Univariate analyses revealed that age, smoking status, T1 slope, C7 slope, and MCs were the risk factors for NP (Table 3). Multivariate analysis was performed to investigate the independent variables on the development of NP. The results show that age (odds ratio [OR], 1.09; 95% confidence interval [CI], 1.02–1.16) and MCs (OR 1.25; 95% CI, 0.09–1.46) were significant independent factors for NP (Table 4).
Discussion
RELATIONSHIP BETWEEN AGE AND NECK PAIN:
Romano et al. [8] reported that older people have a lower pain threshold. They reported that men and women behave differently when it comes to pain, and men are more sensitive to it. Monroe et al. [9] stated that the prevalence of painful conditions increase with age. In our study, the average age of patients with NP (58.1±10.1 years) was higher than patients without NP (42.4±9.1 years). However, this study did not investigate the difference between the sexes for NP sensitivity. Another reason for NP is that degeneration of the cervical spine becomes more severe with age. However, degeneration of the cervical spine is associated with cervical pain. Internal disc disruption (IDD) is a type of cervical degeneration. Cervical disc herniation can compress the nerve root, which can lead NP. Ito et al. [10] stated that IDD accounts for 1% of the causes of NP. Forty percent of lower back pain was attributed to IDD [11]. Videman et al. [12] studied 157 cases of lumbar disc herniation, where the risk of IDD occurrence rate ranged from 0.6% to 0.7% in adults. Older people may almost have IDD, which can press on nerve roots and cause pain, meaning that older people are more likely to have neck pain. Therefore, there must be a correlation between age and NP. There is incidence of NP increased with age. The exact mechanisms for a connection between age and neck pain remains elusive. If the elderly suffer from NP, they should seek medical attention as soon as possible to eliminate cervical spondylosis.
RELATIONSHIP BETWEEN MODIC CHANGES AND NECK PAIN:
Modic change is one of the manifestations of cervical degeneration, showing signal changes of vertebral endplates and subchondral bone on the MRI. De Roos [13] first highlighted it in 1987, describing the signal changes in the lumbar endplate. Thereafter, based on the different signal intensity on MRI, Modic et al. [14] classified the signal changes into types I, II, and III. Type I shows hypointense T1 and hyperintense T2 manifests as bone marrow inflammation and edema; type II shows hyperintense T1 and T2 indicating fatty involution of the marrow and bone; type III shows hypointense T1 and T2 resulting from endplate sclerotic changes (Figure 2). Previous literature has shown a relationship between osphyalgia and MCs [15,16]. Kuisma et al. [17] reported that Modic changes at L5–S1 and Modic type I lesions are more likely to be associated with pain symptoms than other types of Modic changes or changes located at other lumbar levels. Braithwaite et al. [18] did a discography of the disc and found that the sensitivity to pain was 86.7% in the presence of Modic changes and pain sensitivity without MCs was 23.3%. Therefore, lower back pain due to MCs in the lumbar spine is likely related to disc degeneration, which may be discogenic specific changes in low back pain on MRI. This study showed that the incidence of NP in patients with cervical spondylotic disease with Modic changes was higher than that in patients without Modic changes. Our study identified that NP patients with Modic changes type I were more (35.3%), followed by Modic changes type II (22.4%). We believe there is a relationship between cervical MCs and NP, especially type I Modic changes. Many patients with type I Modic changes present with NP. At present, most scholars believe that mechanical compression is not the main cause of lumbago and leg pain, chemical stimulation plays a key role [19]. Peng et al. [20] studied 17 patients with discogenic lower back pain and reported that the nucleus pulposus of the outer ring of fibers along the intervertebral disc fissures, where there is a vascular granulation tissue region have abnormally abundant substance P, prostaglandin E2, and bradykinin, which can lead to pain. Podichetty [21] also found a variety of inflammatory regulators in the discogenic lower back pain intervertebral discs, such as carbon albumin matrix metalloproteinase, prostaglandin E2, tumor necrosis factor and various cytokines, which have been found in degenerative intervertebral discs. Nitric oxide synthase was also reported in the spinal fluid of these patients. We think there are two reasons for Modic changes causing neck pain. First, Modic changes are microfractures that cause mechanical pain. Second, Modic changes produce inflammatory factors that cause pain. These explanations need further investigation.
LIMITATIONS OF THE CURRENT STUDY:
First, Modic changes are rare in the cervical spine; therefore, the sample size is very small. In addition, our conclusion is that age and Modic changes are associated with NP. Further study is required to understand how age and Modic changes cause NP. Finally, this study analyzed the relationship between a finite factor and NP. There may be many other, as yet unidentified factors that influence neck pain.
Conclusions
In cervical spondylosis, age and MCs were associated with NP. When older patients with neck pain seek medical advice as soon as possible, it helps in the early detection of cervical degeneration changes. If the MRI shows Modic changes in patients with neck pain, then neck pain may be caused by Modic changes.
Figures
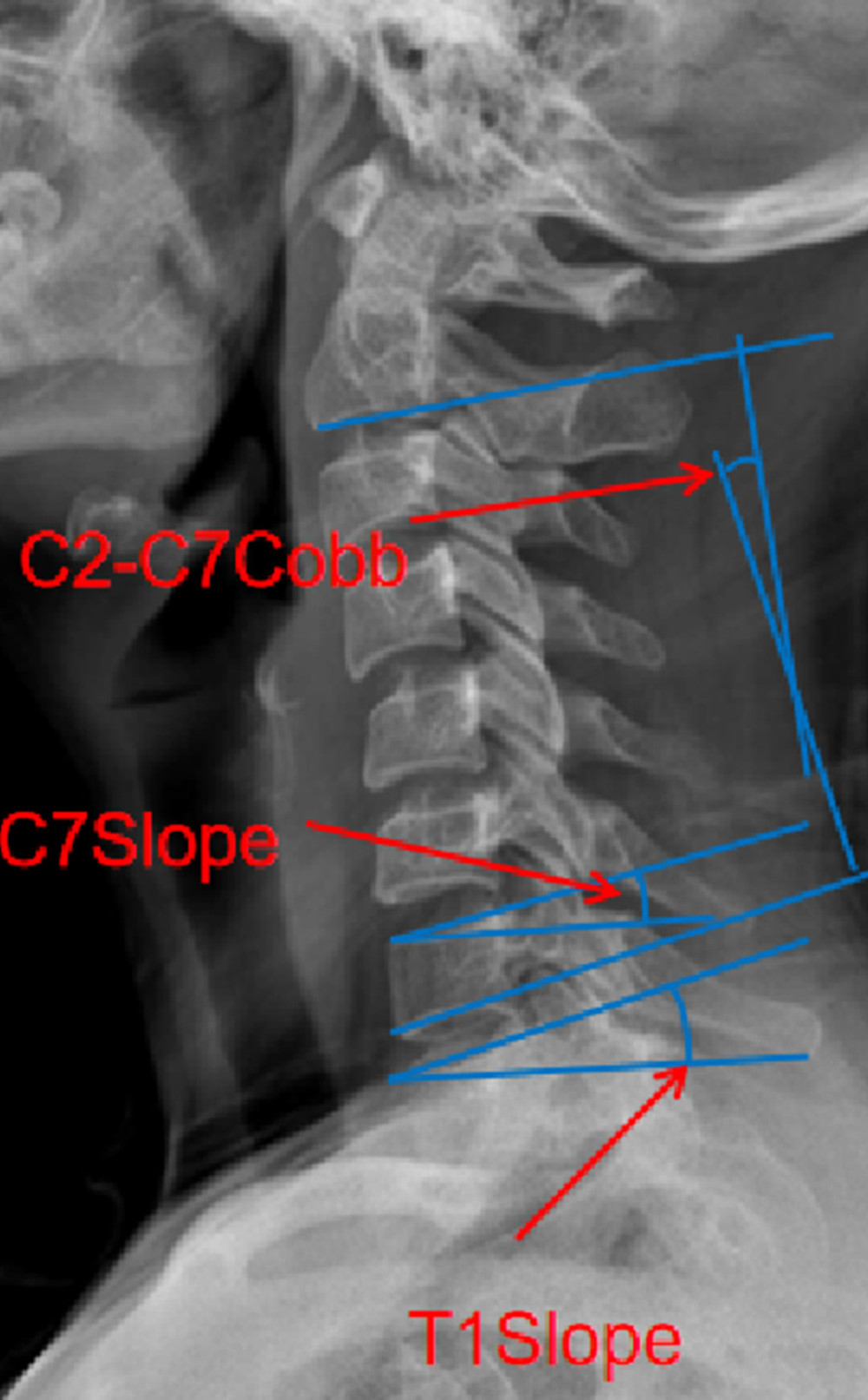 Figure 1. Measurements of the radiological parameters C7 slope, T1 slope, C2–C7 Cobb on a cervical lateral radiograph.
Figure 1. Measurements of the radiological parameters C7 slope, T1 slope, C2–C7 Cobb on a cervical lateral radiograph. 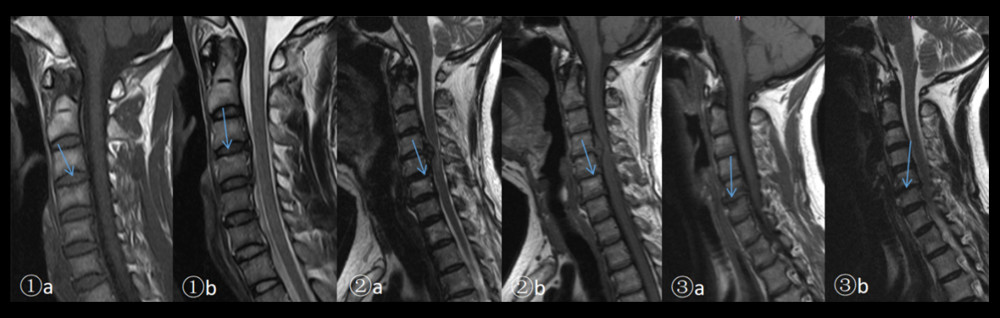 Figure 2. 1a. Modic changes type I: A superior C4 vertebral body showed a lower signal intensity on FSET1WI (arrow). 1b. A superior C4 vertebral body showed a higher signal intensity on frFSE-T2WI (arrow). 2a. Modic changes type II: A superior C6 vertebral body showed high signal intensity on FSE-T1WI (arrow). 2b. A superior C6 vertebral body showed high signal intensity on frFSE-T2WI (arrow). 3a. Modic changes type III: A superior C6 vertebral body showed low signal intensity on FSET1WI (arrow). 3b. A superior C6 vertebral body showed low signal intensity on frFSE-T2WI (arrow).
Figure 2. 1a. Modic changes type I: A superior C4 vertebral body showed a lower signal intensity on FSET1WI (arrow). 1b. A superior C4 vertebral body showed a higher signal intensity on frFSE-T2WI (arrow). 2a. Modic changes type II: A superior C6 vertebral body showed high signal intensity on FSE-T1WI (arrow). 2b. A superior C6 vertebral body showed high signal intensity on frFSE-T2WI (arrow). 3a. Modic changes type III: A superior C6 vertebral body showed low signal intensity on FSET1WI (arrow). 3b. A superior C6 vertebral body showed low signal intensity on frFSE-T2WI (arrow). References
1. Fejer R, Kyvik KO, Hartvigsen J, The prevalence of neck pain in world population: A systematic critical review of the literature: Eur Spine J, 2006; 15(6); 834-48
2. Tsang A, Von Korff M, Lee S, Common chronic pain conditions in developed and developing countries: Gender and age differences and comorbidity with depression-anxiety disorders: J Pain, 2008; 9; 883-91
3. Herman PM, Kommareddi M, Sorbero ME, Characteristics of chiropractic patients being treated for chronic low back and chronic neck pain: J Manipulative Physiol Ther, 2018; 41; 445-55
4. Vos T, Flaxman AD, Naghavi M, Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010: Lancet, 2012; 380; 2163-96
5. Grider JS, Harned M, Cervical spinal cord using monophasic burst waveform for axial neck and upper extremity radicular pain: A preliminary observational study: Neuromodulation, 2019; 34; 212-17
6. Gao X, Li J, Shi Y, Asymmetrical degenerative marrow (Modic) changes in cervical spine: Prevalence, correlative factors, and surgical outcomes: J Orthop Surg Res, 2018; 13; 85
7. Jouibari JF, Le Huec JC, Hameghavandi MH, Comparison of cervical sagittal parameters among patients with neck pain and healthy controls: A comparative cross sectional study: Eur Spine J, 2019; 28(10); 2319-24
8. Romano RR, Anderson AR, Failla MD, Sex differences in associations of cognitive function with perceptions of pain in older adults: J Alzheimers Dis, 2019; 70(3); 715-22
9. Monroe TB, Herr KA, Mion LC, Cowan RL, Ethical and legal issues in pain research in cognitively impaired older adults: Int J Nurs Stud, 2013; 50(9); 1283-87
10. Ito M, Incorvaia KM, Shiwei FY, Predictive signs of discogenic lumbar pain on magnetic resonance imaging with discography correlation: Spine, 1998; 23(11); 1252-58
11. Schwarzer AC, Aprill CN, Derby R, The prevalence and clinical features of internal disc disruption in patients with chronic low back pain: Spine, 1995; 20(17); 1878-83
12. Videman T, Nurminen M, The occurrence of anular tears and their relation to lifetime back pain history: A cadaveric study using barium sulfate discography: Spine, 2004; 29(23); 2668-76
13. de Roos A, Kressel H, Spritzer C, Dalinka M, MR imaging of marrow changes adjacent to endplates in degenerative lumbar disk disease: Am J Roentgenol, 1987; 149(3); 531-34
14. Modic MT, Steinberg PM, Ross JS, Degenerative disk disease: Assessment of changes in vertebral body marrow with MR imaging: Radiol, 1988; 166; 193-99
15. Kong L, Tian W, Cao P, Predictive factors associated with neck pain in patients with cervical disc degeneration: Medicine, 2017; 96(43); e8447
16. Mitra D, Cassar-Pullicino VN, Mccall IW, Longitudinal study of vertebral type-1 end-plate changes on MR of the lumbar spine: Eur Radiol, 2004; 14(9); 1574-81
17. Kuisma M, Karppinen J, Niinimaki J, Modic changes in endplates of lumbar vertebral bodies: Prevalence and association with low back and sciatic pain among middle-aged male workers: Spine, 2007; 32(10); 1116-22
18. Braithwaite I, White J, Saifuddin A, Vertebral end-plate (Modic) changes on lumbar spine MRI: Correlation with pain reproduction at lumbar discography: Eur Spine J, 1998; 7(5); 363-68
19. Alexandre A, Corò L, Azuelos A, Pellone M, Percutaneous nucleoplasty for discoradicular conflict: Acta Neurochir Suppl, 2005; 92; 83-86
20. Peng BG, Wu WW, Hou SXThe pathogenesis of discogenic low back pain: Zhonghua Wai Ke Za Zhi, 2004; 42(12); 720-24 [in Chinese]
21. Podichetty VK, The aging spine: the role of inflammatory mediators in intervertebral disc degeneration: Cell Mol Bill (Noisy-le-grand, France), 2007; 53(5); 4-18
Figures
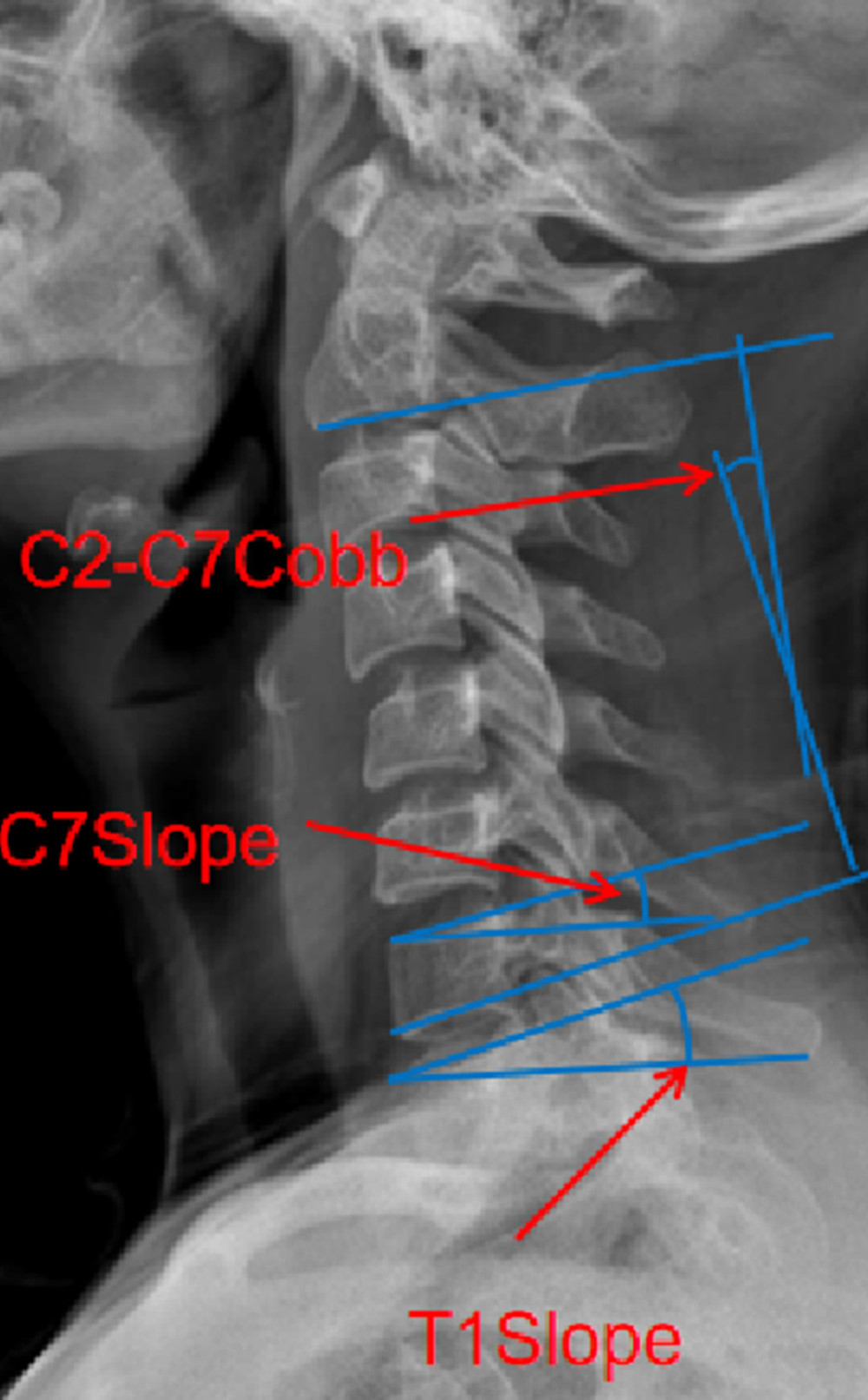 Figure 1. Measurements of the radiological parameters C7 slope, T1 slope, C2–C7 Cobb on a cervical lateral radiograph.
Figure 1. Measurements of the radiological parameters C7 slope, T1 slope, C2–C7 Cobb on a cervical lateral radiograph.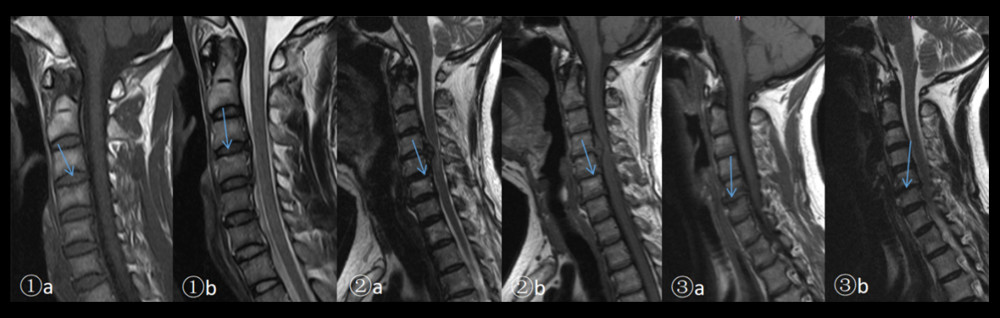 Figure 2. 1a. Modic changes type I: A superior C4 vertebral body showed a lower signal intensity on FSET1WI (arrow). 1b. A superior C4 vertebral body showed a higher signal intensity on frFSE-T2WI (arrow). 2a. Modic changes type II: A superior C6 vertebral body showed high signal intensity on FSE-T1WI (arrow). 2b. A superior C6 vertebral body showed high signal intensity on frFSE-T2WI (arrow). 3a. Modic changes type III: A superior C6 vertebral body showed low signal intensity on FSET1WI (arrow). 3b. A superior C6 vertebral body showed low signal intensity on frFSE-T2WI (arrow).
Figure 2. 1a. Modic changes type I: A superior C4 vertebral body showed a lower signal intensity on FSET1WI (arrow). 1b. A superior C4 vertebral body showed a higher signal intensity on frFSE-T2WI (arrow). 2a. Modic changes type II: A superior C6 vertebral body showed high signal intensity on FSE-T1WI (arrow). 2b. A superior C6 vertebral body showed high signal intensity on frFSE-T2WI (arrow). 3a. Modic changes type III: A superior C6 vertebral body showed low signal intensity on FSET1WI (arrow). 3b. A superior C6 vertebral body showed low signal intensity on frFSE-T2WI (arrow). Tables
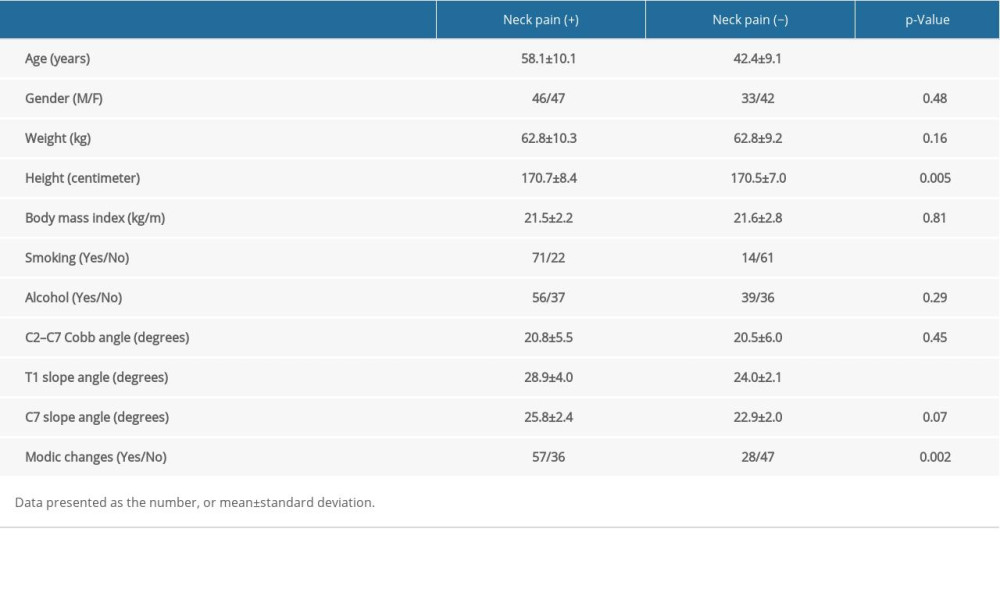 Table 1. Patients’ demographic data and clinical characteristics.
Table 1. Patients’ demographic data and clinical characteristics.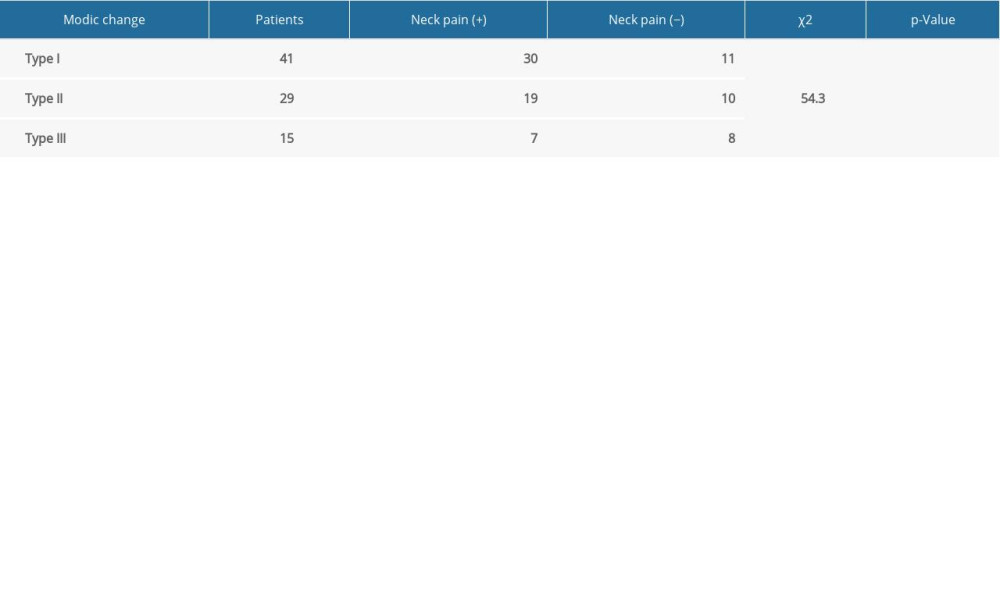 Table 2. Distribution of Modic changes.
Table 2. Distribution of Modic changes. Table 3. Univariate logistic regression analysis of risk factors for neck pain.
Table 3. Univariate logistic regression analysis of risk factors for neck pain.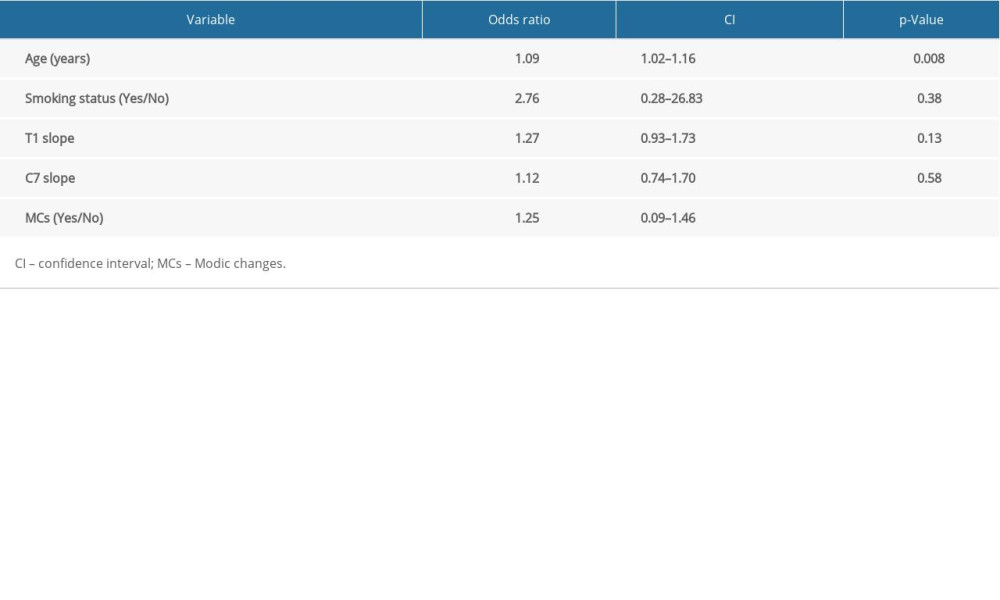 Table 4. Multivariate logistic regression analysis of risk factors for neck pain.
Table 4. Multivariate logistic regression analysis of risk factors for neck pain.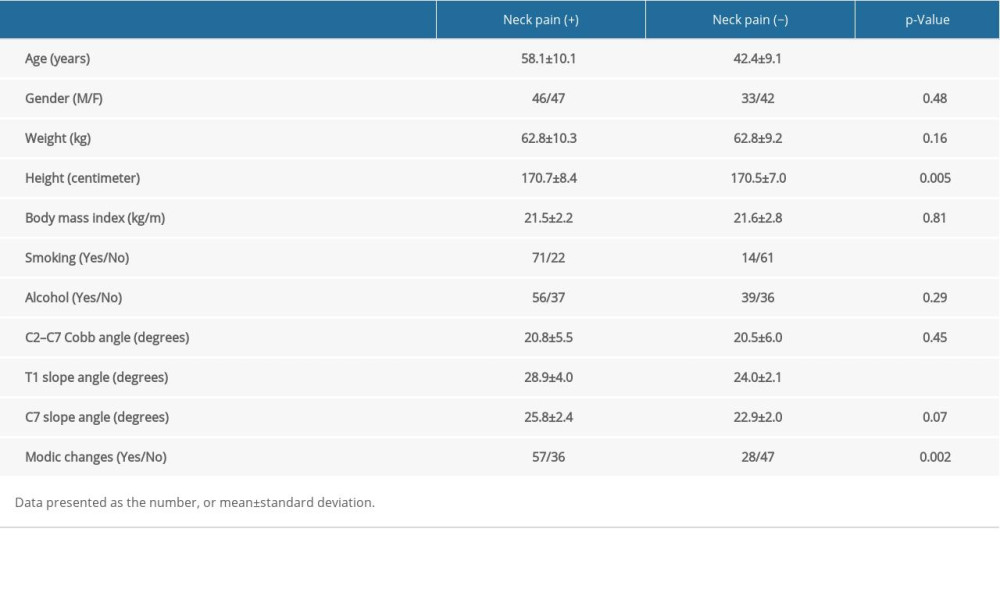 Table 1. Patients’ demographic data and clinical characteristics.
Table 1. Patients’ demographic data and clinical characteristics.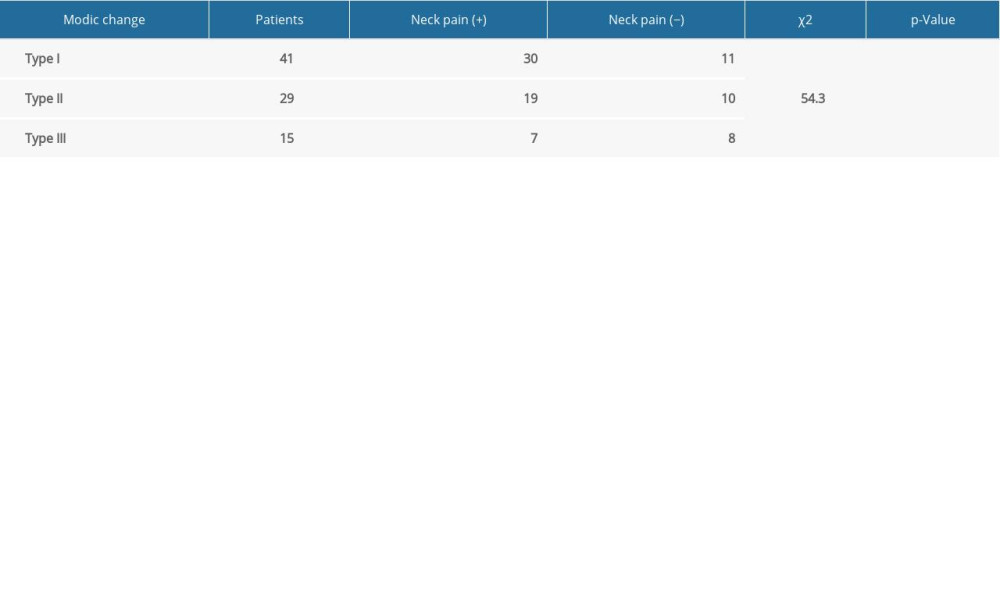 Table 2. Distribution of Modic changes.
Table 2. Distribution of Modic changes. Table 3. Univariate logistic regression analysis of risk factors for neck pain.
Table 3. Univariate logistic regression analysis of risk factors for neck pain.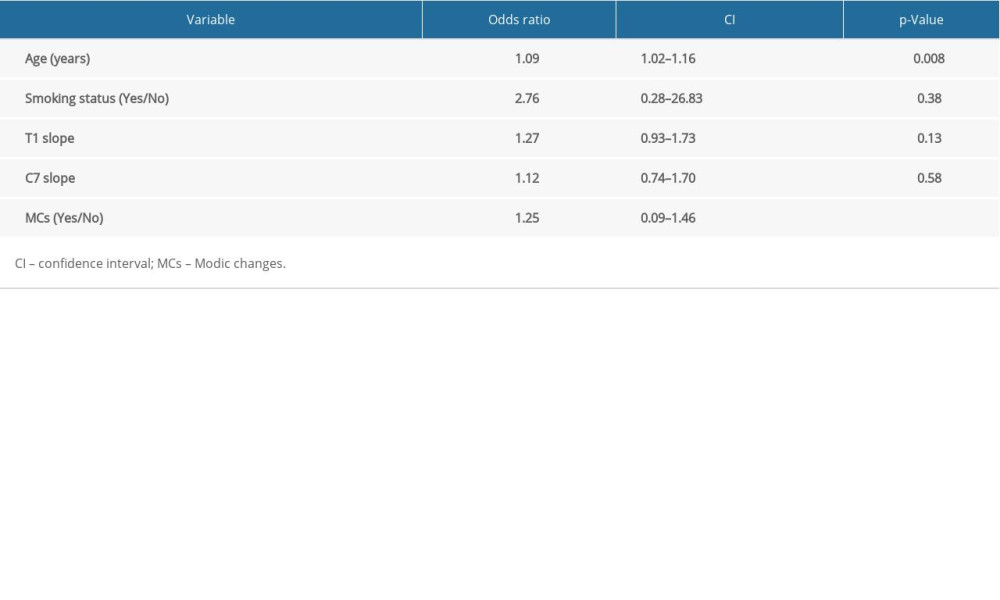 Table 4. Multivariate logistic regression analysis of risk factors for neck pain.
Table 4. Multivariate logistic regression analysis of risk factors for neck pain. In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








