05 September 2023: Articles 
Severe Ketoacidosis After One Anastomosis Gastric Bypass Surgery
Unusual clinical course, Challenging differential diagnosis, Diagnostic / therapeutic accidents, Management of emergency care, Clinical situation which can not be reproduced for ethical reasons
Nadav Nevo1BF, Giuseppe Evola2E, Carlo Sagnelli3E, Niv Pencovich1B, Gabriele Carbone3E, Corrado Rispoli3BDOI: 10.12659/AJCR.939581
Am J Case Rep 2023; 24:e939581
Abstract
BACKGROUND: Bariatric surgeries, such as one anastomosis gastric bypass (OAGB), has become a popular treatment option for managing obesity and associated comorbidities, including type-2 diabetes mellitus (T2DM). However, severe starvation ketoacidosis is a rare but potentially life-threatening complication that can occur postoperatively in patients with T2DM. Despite the increasing prevalence of these surgeries, the existing literature has limited information on severe starvation ketoacidosis as a postoperative complication. It is essential for healthcare professionals to be aware of this complication, its manifestations, and risk factors to ensure patient safety and improve outcomes. Therefore, this article aims to address the current gap in the literature and provide a comprehensive review of severe starvation ketoacidosis as a postoperative complication of bariatric surgeries, specifically OAGB, and its associated risk factors and manifestations.
CASE REPORT: A 38-year-old man with severe obesity and inadequately managed T2DM underwent OAGB surgery. On the second postoperative day, the patient experienced severe starvation ketoacidosis, exhibiting symptoms such as drowsiness, fatigue, weakness, and Kussmaul breathing. Blood gas analysis indicated significant metabolic acidosis. He was quickly transferred to the Intensive Care Unit (ICU) and given intravenous glucose and insulin therapy. Following this intervention, he showed rapid recovery and normalization of blood gases. He was discharged 6 days after surgery with normal clinical examination results and laboratory indices.
CONCLUSIONS: This case study emphasizes the significance of thorough preoperative glycemic control, comprehensive perioperative multidisciplinary management, and close postoperative monitoring for diabetic patients undergoing metabolic and bariatric surgeries. By implementing these strategies, healthcare professionals can reduce the risk of complications such as hypoglycemia or hyperglycemia/diabetic ketoacidosis (DKA) and enhance patient outcomes. The case also highlights the need for continuous education and training for healthcare providers to identify and manage such rare complications effectively.
Keywords: Bariatric Surgery, Starvation, Male, Humans, Adult, Gastric Bypass, Diabetes Mellitus, Type 2, Diabetic Ketoacidosis, Obesity
Background
Metabolic and bariatric surgery such as one anastomosis gastric bypass (OAGB) has become increasingly popular in managing obesity and its associated medical problems, such as type 2 diabetes mellitus (T2DM) [1,2]. However, diabetic ketoacidosis (DKA) is a rare but potentially life-threatening complication following these procedures. DKA is typically characterized by hyperglycemia, acidosis, and ketonuria, and its risk factors and manifestations vary across patients. In the current literature, there is limited information about the occurrence of DKA after metabolic and bariatric surgery, particularly in the context of severe starvation ketoacidosis. Starvation ketoacidosis can result from prolonged fasting or inadequate caloric intake [3–7] and adds an additional layer of complexity to the management of postoperative complications. This case report presents a unique instance of severe starvation ketoacidosis in a patient with T2DM following one anastomosis gastric bypass (OAGB) surgery, adding valuable insights to the existing knowledge on this rare complication.
Case Report
A 38-year-old man with severe obesity (weight 113 kg, height 177 cm, body mass index 36.1) and a history of type-2 diabetes mellitus (T2DM) was scheduled for a one anastomosis gastric bypass (OAGB). He was diagnosed with T2DM 8 years prior and was prescribed daily Glucophage treatment combined with insulin therapy. Unfortunately, he was non-compliant with insulin therapy and adhered only to daily Glucophage treatment. Consequently, his glycated hemoglobin (HbA1C) level reached 13.2% 2 months before surgery. Due to his uncontrolled diabetes and low compliance with prescribed medical treatments, the endocrinologist recommended bariatric surgery to achieve better diabetes control.
A preoperative workup revealed mild gastroesophageal reflux and fatty liver. Apart from T2DM, the endocrinological evaluation was unremarkable. The patient was advised to maintain a normal diet before surgery but reported a low-calorie intake for several days preoperatively.
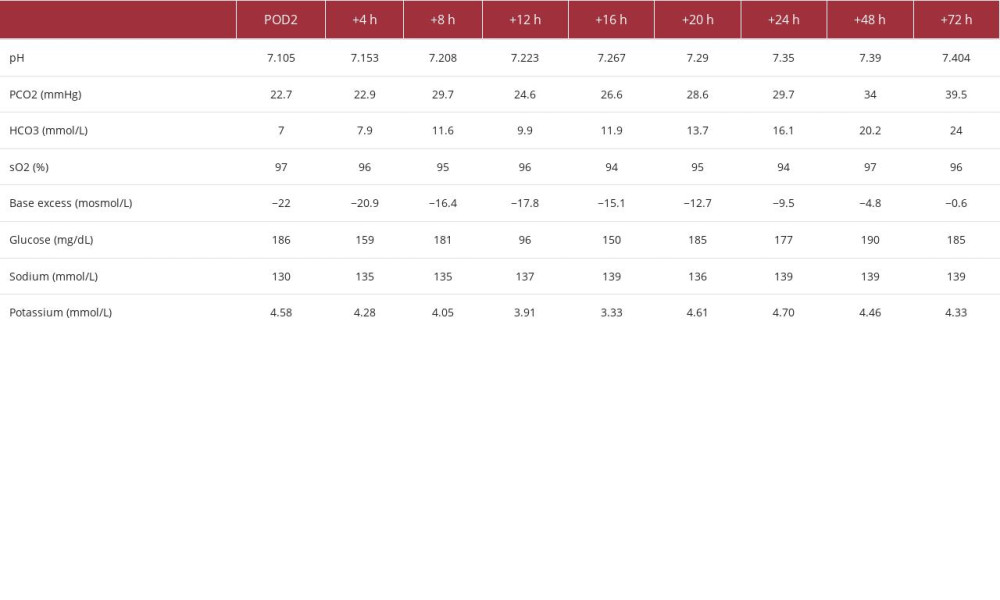
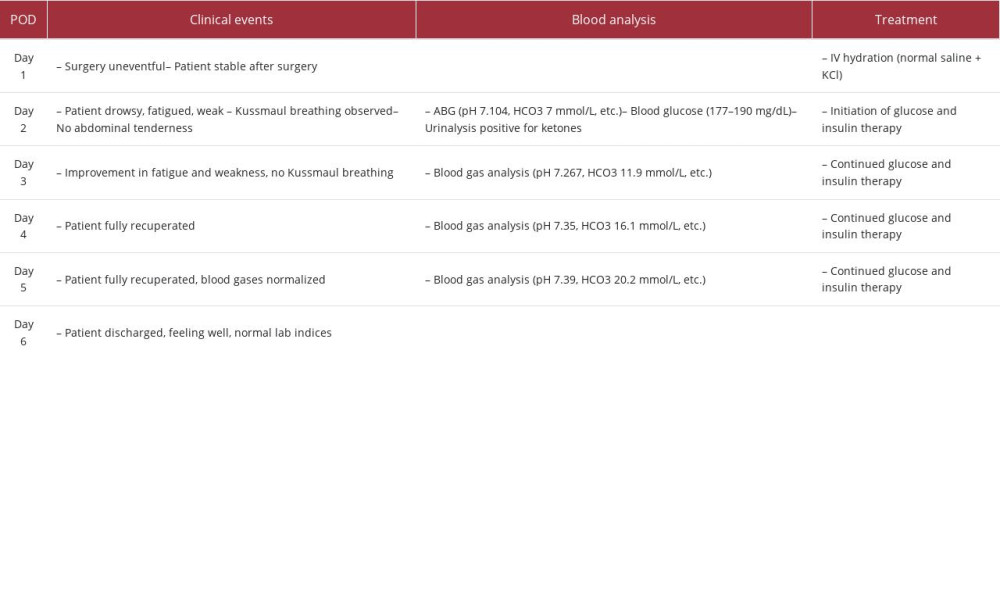
The OAGB surgery was uneventful, and the patient was hydrated with intravenous normal saline supplemented with potassium chloride postoperatively. As in every surgical procedure requiring fasting, his oral anti-diabetic agents were suspended during the postoperative fasting period, and glycemic levels were closely monitored. On postoperative day 2 (POD2), he exhibited drowsiness, fatigue, and weakness, with Kussmaul breathing, but no abdominal tenderness. Arterial blood gas analysis revealed severe metabolic acidosis (pH 7.104, HCO3 7 mmol/L), while blood glucose was 161 mg/dL, and urinalysis showed ketones (+++). Other laboratory values were within normal limits, including electrolytes, blood count, and renal function (Table 1).
The patient was transferred to the intensive care unit for intravenous glucose and insulin treatment, rapidly recovering and with normalizing blood gases. Six days after surgery, he was discharged home, feeling well and with normal clinical and laboratory findings (Table 2).
Discussion
High anion gap metabolic acidosis can be primarily attributed to 5 causes: ketoacidosis, lactic acidosis, ingestions, renal failure, and massive rhabdomyolysis [8]. Ketoacidosis can be induced by uncontrolled diabetes mellitus, alcohol consumption, or fasting. Uncontrolled diabetes mellitus is the most common cause of ketoacidosis, almost always presenting with hyperglycemia consisting of blood glucose concentration exceeding 250 mg/dL and usually much higher [9,10].
In this case, the patient presented with normal blood lactate levels, normal kidney functions, no signs or history of ingestions, and normal blood CPK levels. These parameters and the documented high level of urine ketones point toward ketoacidosis. The patient’s blood glucose levels remained under 200 mg/dL during admission and were uneventful the first 2 days after surgery, suggesting starvation ketoacidosis as the leading diagnosis.
Overproduction of ketoacids, leading to metabolic acidosis, requires both an insulin deficiency-associated increase in the delivery of fatty acids to the liver due to enhanced lipolysis and a resetting of hepatocyte function so that free fatty acids are preferentially converted to ketoacids rather than triglycerides, caused by excess glucagon [11]. The lack of carbohydrate in-take associated with starvation can establish the appropriate hormonal settings, low insulin, and high glucagon, leading to ketosis [12]. However, unlike the severe ketoacidosis that can occur in uncontrolled diabetes, the blood level of ketoacids is usually limited with fasting, potentially due to the promotion of insulin secretion by ketonemia, resulting in limited availability of free fatty acids [9]. In obese patients, these regulatory mechanisms are often deranged [4,12].
Our patient developed severe starvation ketoacidosis 2 days after surgery. He was maintained on IV normal saline with potassium chloride without carbohydrate supplements while fasting following surgery, as are many of our bariatric surgery patients. A potential explanation for this rapid and acute course is the patient’s preoperative HbA1C level of 13.2%, which suggests ongoing uncontrolled diabetes mellitus, likely with both type 1 and type 2 components. Elevated glucagon secretion following surgery and fasting challenged the chronic low insulin levels and exhausted glycogen stores. In this case, augmented insulin secretion could not be produced in response to ketonemia, resulting in uncontrolled severe ketoacidosis.
Conclusions
This case report emphasizes the crucial need for careful peri-operative management of diabetic patients undergoing one anastomosis gastric bypass (OAGB) surgery, with particular attention given to the prevention and early recognition of severe starvation ketoacidosis. Good glycemic control preoperatively and close monitoring in the immediate postoperative period are necessary to prevent severe metabolic derangements. The involvement of a multidisciplinary team, including endocrinologists, dieticians, and surgical teams, is essential to optimize outcomes and prevent severe complications. This report serves as a reminder of the importance of preoperative counseling and tailored management to mitigate the risks associated with metabolic and bariatric surgery.
References:
1.. De Luca M, Piatto G, Merola G, IFSO update position statement on one anastomosis gastric bypass (OAGB): Obesity Surgery, 2021; 31(7); 3251-78
2.. Kermansaravi M, Parmar C, Chiappetta S, Patient selection in one anastomosis/mini gastric bypass – an expert modified Delphi consensus: Obes Surg, 2022; 32(8); 2512-24
3.. Foster DW, McGarry JD, The metabolic derangements and treatment of diabetic ketoacidosis: N Engl J Med, 1983; 309(3); 159-69
4.. Reichard GA, Owen OE, Haff AC, Ketone-body production and oxidation in fasting obese humans: J Clin Invest, 1974; 53(2); 508-15
5.. Lulsegged A, Saeed E, Langford E, Starvation ketoacidosis in a patient with gastric banding: Clin Med (Lond), 2011; 11(5); 473-75
6.. Valkenborgh T, Bral P, Starvation-induced ketoacidosis in bariatric surgery: A case report: Acta Anaesthesiol Belg, 2013; 64(3); 115-17
7.. Bruegger D, Rehm M, Da Silva L, Severe metabolic acidosis resulting from a dislocated gastric band: Obes Surg, 2004; 14(4); 555-58
8.. Gabow PA, Kaehny WD, Fennessey PV, Diagnostic importance of an increased serum anion gap: N Engl J Med, 1980; 303(15); 854-58
9.. Trachtenbarg DE, Diabetic ketoacidosis: Am Fam Physician, 2005; 71(9); 1705-14
10.. Eledrisi MS, Alshanti MS, Shah MF, Overview of the diagnosis and management of diabetic ketoacidosis: Am J Med Sci, 2006; 331(5); 243-51
11.. Cahill GF, Fuel metabolism in starvation: Annu Rev Nutr, 2006; 26; 1-22
12.. Umpierrez GE, Smiley D, Kitabchi AE, Narrative review: ketosisprone type 2 diabetes mellitus: Ann Intern Med, 2006; 144(5); 350-57
In Press
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250