29 July 2023: Articles 
Botulinum Toxin as an Adjunctive Therapy for Immobilization of a Distal Humerus Fracture in Parkinson’s Disease-Associated Psychosis: A Case Report
Unusual clinical course, Unusual or unexpected effect of treatment
Justin Lapow1EF*, Jacob Hirth1EF, Avinesh Agarwalla2AEF, David S. WellmanDOI: 10.12659/AJCR.939680
Am J Case Rep 2023; 24:e939680
Abstract
BACKGROUND: Attainment of extremity immobilization in orthopedic trauma patients experiencing psychosis is often uniquely challenging. Many fractures, including those of the distal humerus, require a period of immobilization postoperatively to optimize fracture healing. Patients with Parkinson's disease have also been shown to have lower rates of union after fracture compared to the general population. The combination of Parkinson's disease and associated psychosis requires heightened attention to those parameters that may hinder fracture healing, such as inadequate immobilization of the fracture. Botulinum toxin has previously been described as a potential adjunctive therapy for fracture immobilization but has not yet been described in the setting of distal humerus fractures.
CASE REPORT: A 75-year-old woman with Parkinson's disease-associated psychosis presented 2 weeks after open reduction and internal fixation of a distal third humeral shaft fracture due to failure of fixation and episodes of violent hallucinations. The patient underwent irrigation and debridement, and revision open reduction and internal fixation. Given her uncontrolled hallucinations, intramuscular botulinum toxin injections were given to the right triceps, biceps, and brachialis muscles to aid in the immobilization of the right extremity and protect the surgical site during the perioperative period. The patient subsequently followed up at the clinic 3 months postoperatively with ongoing fracture healing, evidenced by bridging callous and bone formation on radiographs, as well as a return of motion to the extremity.
CONCLUSIONS: Botulinum toxin may be a safe and effective adjunct for fracture immobilization in patients who are difficult to immobilize and have high fixation failure risk.
Keywords: Botulinum Toxins, Type A, humeral fractures, Immobilization, Orthopedic Procedures, Psychotic Disorders, Female, Humans, Aged, Humeral Fractures, Distal, Parkinson Disease, Treatment Outcome, Hallucinations
Background
Humeral shaft fractures account for 1–5% of all fractures, with an incidence of about 13 cases per 100 000 persons per year [1,2]. Of these, 10–20% involve the distal humeral shaft [3,4]. Patients with orthopedic injuries and concomitant psychiatric illness are at a greater risk for postoperative morbidity and mortality [5,6]. Parkinson’s disease (PD) is a common neurologic condition that is associated with psychosis in 16% to 75% of patients [7]. Previously, the psychotic symptoms associated with PD were believed to be the result of the dopaminergic medications used for treatment of the disease [8]. More recently though, PD-associated psychosis has been recognized as having a multifactorial etiology, with sleep disorders, cognitive impairment, and the alterations in neurochemistry that result from PD itself, all being implicated [7,8]. The psychosis associated with PD is characterized by visual hallucinations and has been linked to an increased utilization of long-term care and mortality risk [8,9]. PD has also been identified as an independent risk factor for delirium, which must be differentiated from psychosis during the management of PD [7,10,11]. Unlike PD-associated psychosis, delirium generally results from reversible causes. Infections, trauma, sepsis, and surgery are all known causes of delirium, especially in the setting of PD [11]. Medical illnesses, such as infections, often trigger the initial presentation of psychosis or can result in an exacerbation of preexisting psychosis in PD patients [7]. Thus, the interplay between psychosis and delirium in PD is complex and often challenging for healthcare providers.
PD patients have been shown to have almost twice the risk for falls and fractures as those without PD [12]. Patients with PD-associated psychosis have a modest consistent annual increase in fall and fracture risk compared to PD patients without psychosis [13]. Additionally, PD patients experience treatment failure (eg, nonunion, malunion) at a rate of 40.5%, which is higher than the general population at 0.2–24% [14]. Following initial conservative management, only 33.3% of patients with significant psychiatric history achieve union in under 26 weeks, while 67% of patients with psychiatric history achieve union during the same interval following operative intervention [15]. Conservative management may result in less favorable outcomes due to difficulties associated with brace care and compliance, coupled with the burden of psychiatric illness [15].
Botulinum toxin injection has been previously described as a potential immobilization technique for fractures when injections are made into muscles that cross the fracture site or those that could produce excessive strain forces on the fracture if not adequately immobilized. Previous literature has shown favorable outcomes following botulinum toxin-induced immobilization in numerous fractures, including those of the clavicle, mandible, scapula, and femur [16–23]. To the best of our knowledge, this is the first report of botulinum toxin assisted immobilization of a distal humerus fracture in a PD patient with psychosis.
Case Report
A 75-year-old right-hand-dominant woman with a past medical history of PD and associated psychosis presented to the Emergency Department with a right distal third humerus fracture that was sustained after a ground level fall due to weakness while at the nursing facility in which the patient resided (Figure 1). Her PD symptoms primarily consisted of resting tremor and rigidity, along with unsteadiness during ambulation. The patient’s outpatient PD management was with 100 mg of amantadine nightly, as well as 118.75–475 mg of carbidopa-levodopa every 3 hours. Although she had a known history of PD-associated psychosis, she was alert and oriented but forgetful at the time of initial presentation to the hospital. Open reduction and internal fixation of the humerus fracture was indicated due to the patient’s desire for functional optimization, as well as the degree of displacement of the fracture segments after reduction (Figure 2). The patient was subsequently brought to the operating room for an ORIF of the fracture. The patient was placed in the supine position on the operating room table, general anesthesia was administered along with preoperative cefazolin, and the right upper extremity was prepped and draped in the standard fashion. A posterior approach to the humerus with Gerwin modification was performed. The radial nerve was identified followed by reflection of the triceps muscle from lateral to medial. Once the radial nerve and surrounding structures were mobilized and dissected free to allow for plating, the fracture was identified. Reduction of the fracture was performed with clamps and a 2.7-mm plate was placed over the lateral aspect of the humerus. Proximal and distal screws were placed to hold the reduction. A 3.5-mm plate was then atraumatically slid under the radial nerve. Cortical screws were placed proximally and distally to bring the plate flush with bone. Clamps were then used to optimize reduction. Interfragmentary compression screws were placed in the 3.5-mm plate from posterior to anterior. A combination of cortical and locking screws were then used to fill the remainder of each plate. Of note, locking screws were utilized in many of the distal holes secondary to poor bone quality. None of the proximal screws were placed in locking fashion, as each had acceptable diaphyseal purchase. Wounds were then copiously irrigated, and the incision was closed in the standard fashion with a deep drain left in place. The right upper extremity was placed in a splint and the patient was awoken from anesthesia. Postoperatively, the patient had intact motor and sensory function of the median, ulnar, and radial nerves.
Postoperatively, she was found to have altered mental status and underwent a workup for infectious etiologies, including urinalysis, urine culture, chest X-ray, complete blood count, and blood culture, which all were negative for findings consistent with infection. The patient also underwent a CT scan of the head without contrast that found no evidence of hemorrhage, mass effect, or midline shift. She was determined to have altered mental status secondary to post-surgical delirium. Her delirium resolved with continuation of her home medications and other non-pharmacologic measures. She was then discharged to a nursing home on postoperative day 5. At the time of discharge, her mental status had returned to baseline, she had been mobilized by physical therapy, and she was advised to continue with non-weight bearing of the right upper extremity with a sling.
On postoperative day 15, she returned to the hospital and was found to have skin breakdown over the posterolateral incision and refracturing of the distal humerus, which occurred secondary to an altered mental status with violent hallucinations (Figure 3). She presented with agitation, apparent visual hallucinations, and episodes of forceful thrashing motions of the upper extremities. The reinjury of her right humerus was caused by her striking the extremity on a bedrail during an episode of hallucinations at the nursing facility. A full assessment of the patient’s worsened mental status was conducted by the Emergency Department and Neurology Team, including urinalysis, complete blood count, chest X-ray, and a non-contrast CT scan of the head. Blood and urine cultures were also sent to the laboratory for analysis at that time. After the workup, it was determined that she was experiencing an exacerbation of PD-associated psychosis. Due to the concern for a now open distal humerus fracture, she was given a tetanus booster and dose of cefazolin in the Emergency Department. She was then brought to the operating room for irrigation and debridement, implant removal, and revision ORIF.
The patient was placed in the lateral position and general anesthesia was administered. Preoperative antibiotics were initially held in anticipation of obtaining intraoperative wound cultures. Her previous operative incision was opened, and dissection was carried down to the humerus through the lateral window of the paratricipital approach, while identifying and protecting the radial nerve. The previous implants were removed, and 5 cultures were taken. Extensive irrigation and debridement of the wound and fracture site was performed due to the presence of wound breakdown. Antibiotics were administered at this time. Following this, it was determined that the medial window of the paratriciptal approach was needed to treat what was now a T-condylar humerus fracture. A full neuroplasty of the ulnar nerve was performed. The medial column was reduced first due to the higher degree of comminution within the lateral column. Once reduction of the medial column was achieved, a 2.4-mm plate was placed over the posterior aspect of the humerus with 2 unicortical locking screws placed proximally and distally to provisionally secure the reduction. Large pieces of comminuted bone were reduced back to the stable medial column, and the long medial plate was then placed, avoiding the ulnar nerve. A long lateral plate was slid under the radial nerve, with care taken to avoid nerve compression, and cortical screws were used proximally and distally to bring the plate flush with bone. A mixture of cortical and locking screws completed the construct, secondary to the poor bone stock (Figure 4). The incision was closed in standard fashion. Sterile dressings were applied, and the arm was immobilized with a splint. Motor and sensory function was confirmed to be intact in the radial, median, and ulnar nerves.
Postoperatively, the patient was found to have ongoing altered mental status with agitation and visual hallucinations. The Neurology Team was consulted for continued management of the patient’s PD and altered mental status. Her PD was treated with continuation of her home dosing of amantadine and carbidopa-levodopa, while the altered mental status was managed with 12.5 mg of oral haloperidol as needed. On postoperative day 1, we held a discussion with the Neurology Team regarding the administration of botulinum toxin injections in the flexor and extensor muscles of the elbow to help immobilize the fracture given the patient’s ongoing psychosis. After discussion of the risks and benefits with all involved parties, the Neurology Team proceeded with the injections. It was determined that injections into the biceps, triceps, and brachialis muscles would provide adequate immobilization of the elbow, while still preserving fine motor function of the hand. The deltoid muscle was spared, as the fracture did not extend past the deltoid tuberosity. This also helped prevent excessive deltoid muscle atrophy and shoulder stiffness. We reconstituted 200 units of botulinum toxin (OnabotulinumtoxinA) in 8 cc normal saline; this dilution of botulinum toxin was determined by the Neurology Team to be adequate for providing an optimal dosage to each of the intended injection sites. Using EMG guidance, 100 units were injected in the right triceps in 4 sites, 75 units were injected in the biceps in 2 sites, and 25 units were injected into the brachialis. Resolution of the patient’s psychiatric symptoms was ultimately achieved in the subsequent days with continued medical management and collaboration with Neurology. The patient was discharged to a nursing home on postoperative day 13 and had no further hospitalizations for psychiatric symptoms in the follow-up period. She had no active flexion or extension at the elbow at this time. The elbow was maintained at 90 degrees in a cast.
She followed up in the office at 3 months postoperatively with no evidence of wound breakdown, drainage, or infection. Her pain was well-controlled at that time. X-rays (Figure 5) showed clear callous formation and bridging bone across the fracture, indicating that fracture healing was occurring. No loss of reduction or hardware concerns were observed on the radiographs. Motor and sensory function was intact in the median, radial, and ulnar nerves. Muscle function was 4-/5 strength in the right triceps and biceps. Range of motion testing showed a 45-degree arc of flexion and extension through the elbow. The patient was cleared to continue range of motion of her elbow and utilize a sling as necessary for pain control. However, the patient died before the next follow-up appointment due to unrelated causes.
Discussion
ORIF is the mainstay treatment for distal humerus fractures. However, elderly patients have higher risk of adverse outcomes than younger patients [24]. Careful evaluation and management is required for elderly patients due to suboptimal rehabilitation capacity, low physiologic reserve, complex intra-articular comminution, and poor soft-tissue and bone quality [24]. Furthermore, PD patients have been shown to have a greater risk for osteoporosis, which can increase fracture susceptibility and impact healing [25]. Figueroa and Rosen posited that the lower bone mineral density in PD patients may be due to a combination of the following factors: dysregulation of the autonomic nervous system’s ability to control skeletal homeostasis, direct inhibition of osteoclast and osteoblast function by levodopa, increased prevalence of sarcopenia, hormonal alterations, and low levels of vitamin D [25]. The increased muscle tone and tremors observed in PD patients have been implicated in fracture destabilization [14]. ORIF enables an accelerated return to motion, reducing the risk of complications associated with prolonged immobilization [26]. The distal humerus is subjected to a high degree of mechanical stress during functional recovery, necessitating a rigid and durable internal fixation [24]. Failure of fixation can occur if sufficient stabilization is not achieved with the limited bone stock.
The unstable nature of the original fracture, along with the patient’s psychiatric status, required additional fracture immobilization strategies beyond splinting to optimize healing. In the revision case, the use of botulinum toxin allowed for temporary, strategic paresis of the appropriate muscles to ensure adequate immobilization occurred, which then facilitated union of the fracture. Although botulinum toxin injections gained their notoriety for cosmetic applications, botulinum toxin has become an increasingly popular treatment modality for a wide array of medical conditions, with applications ranging from migraine prophylaxis to spasticity reduction in patients with cerebral palsy or stroke [27,28].
Botulinum toxin blocks acetylcholine release from the skeletal and autonomic presynaptic nerve terminals through inhibition of normal vesicle-plasma membrane fusion [29]. This occurs through interactions with the soluble N-ethylmaleimide sensitive factor attachment protein receptors (SNARE or SNAP receptors) that normally function to facilitate vesicle release [27]. When injected into skeletal muscle, botulinum toxin can induce paralysis of the muscle that lasts for 3–4 months [29]. This duration of action makes botulinum toxin a drug of interest for fracture immobilization in patients that require additional prolonged abstinence from motion during the first 3 months of healing.
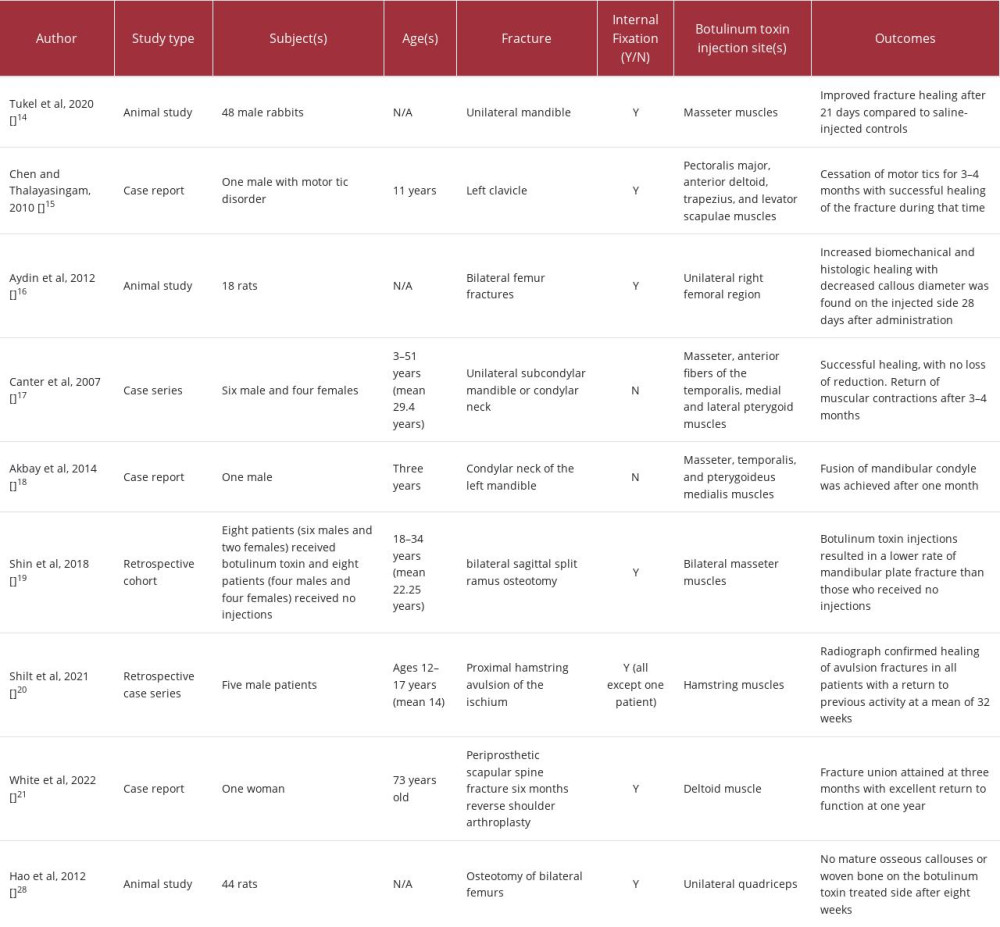
Numerous studies have described the successful use of botulinum toxin in the treatment of mandibular fractures [19–21]. White et al described the use of botulinum toxin as an adjunct therapy in a case of a periprosthetic scapular spine fracture, whereby the botulinum toxin was injected into the deltoid muscle to reduce potential strain from the muscle on the surrounding fracture site [23]. Chen and Thalayasingam reported a case of botulinum toxin use in a child with a clavicular fracture and motor tic disorder to control the pain at the fracture site caused by the tics, as well as provide adequate immobilization of the fracture for healing [17]. In a case series by Shilt et al, botulinum toxin was utilized in 5 male patients to achieve controlled immobilization and prevention of tendon repair failure following proximal hamstring avulsion repair [22]. In animal models, botulinum toxin has been used to improve fracture healing when injected into surrounding muscles in femoral and mandibular fractures [16,18]. Conversely, Hao et al demonstrated that botulinum toxin injections in the quadriceps muscles of rats with femur fractures resulted in muscle atrophy and instability that impaired callous maturation and union at 8 weeks postoperatively [30] (Table 1). Further understanding is still needed regarding the dosage required for efficacy and the potential influence of botulinum toxin on the physiologic processes associated with fracture healing. It is plausible that highly unstable fractures or those that occur in certain locations, such as near or involving a joint, where motion may occur, could benefit from the additional immobilization provided by botulinum toxin injections into the surrounding musculature. However, botulinum toxin-induced immobilization may not provide additional benefits for fractures when the conditions for adequate fracture healing are easily obtained through standard reduction and immobilization techniques and instead, the benefits may be outweighed by the potential for muscle atrophy and stiffness. The use of botulinum toxin may also be beneficial when medical, social, or psychiatric conditions hinder a patient’s ability to comply with immobilization protocols.
There is currently a dearth of literature evaluating the utility of botulinum toxin for immobilization of upper extremity fracture. The case presented herein suggests botulinum toxin is an effective adjunct for fracture immobilization in difficult to manage patients with high fixation failure risk. This patient’s active hallucinations made adequate postoperative immobilization challenging, resulting in initial fixation failure. Immobilization beyond splinting and casting was necessary following revision surgery to prevent further complications and salvage the limb. Botulinum toxin was utilized following revision ORIF to minimize the risk of an additional fixation failure. Injections were made in the muscles primarily responsible for elbow flexion and extension, namely the biceps, triceps, and brachialis. This induced paralysis of only those muscles that cross the elbow and prevented active flexion or extension of the elbow joint, while still preserving function of the hand. Immobilization of the patient’s shoulder joint was not required in this case because the fracture was limited to the distal third of the humerus and did not extend to the proximal humerus. Immobilization of the elbow with botulinum toxin helped to protect the fracture and fixation construct from motion and stress forces that may have resulted if the patient were to have continued uncontrolled movement of the extremity during episodes of psychosis. Furthermore, we did not observe any adverse effects of botulinum toxin on fracture healing in our patient. The induced paralysis of the elbow flexor and extensor muscles may have also aided in reducing the musculoskeletal manifestations of PD that could adversely affect fracture healing, such as tremor, rigidity, or dystonia. Botulinum toxin is only a temporary, local paralytic, which allowed the patient to regain motion in the affected arm after 3 months and enabled sufficient time to achieve enough bony union to allow for traditional rehabilitation (ie, range of motion and strength) to begin. Although the patient died before the long-term benefit of this approach could be fully assessed, the follow-up radiographic and physical examination findings indicate that a favorable outcome was achieved. Collaboration with Neurology was imperative in this case to optimize the management of this complex patient, as Neurology aided in the management of the patient’s mental status and administration of botulinum toxin injections.
Conclusions
Botulinum toxin may be a safe and effective adjunct for upper-extremity immobilization in patients with distal humerus fractures who are difficult to immobilize using standard methods of casting or splinting and have high fixation failure risk. Botulinum toxin may be particularly useful in patients with PD-associated psychosis when the patient’s mental status may impair the attainment of sufficient immobilization for fracture healing. Immobilization of the injured upper extremity with botulinum toxin was performed without any apparent adverse effects on fracture healing. The patient regained active motion of the extremity 3 months after botulinum toxin administration.
Figures
References:
1.. Gallusser N, Barimani B, Vauclair F, Humeral shaft fractures: EFORT Open Rev, 2021; 6(1); 24-34
2.. Court-Brown CM, Caesar B, Epidemiology of adult fractures: A review: Injury, 2006; 37(8); 691-97
3.. Tsai CH, Fong YC, Chen YH, The epidemiology of traumatic humeral shaft fractures in Taiwan: Int Orthop, 2009; 33(2); 463-67
4.. Tytherleigh-Strong G, Walls N, McQueen MM, The epidemiology of humeral shaft fractures: J Bone Joint Surg Br, 1998; 80(2); 249-53
5.. Brown A, Alas H, Bortz C, Patients with psychiatric diagnoses have increased odds of morbidity and mortality in elective orthopedic surgery: J Clin Neurosci, 2021; 84; 42-45
6.. Schwartz S, Bazargan-Hejazi S, Pan D, Association of psychiatric diagnostic conditions with hospital care outcomes of patients with orthopedic injuries: Perm J, 2018; 22; 17-120
7.. Chang A, Fox SH, Psychosis in Parkinson’s disease: Epidemiology, pathophysiology, and management: Drugs, 2016; 76(11); 1093-118
8.. Fredericks D, Norton JC, Atchison C, Parkinson’s disease and Parkinson’s disease psychosis: A perspective on the challenges, treatments, and economic burden: Am J Manag Care, 2017; 23(5 Suppl.); S83-S92
9.. Wetmore JB, Li S, Yan H, Increases in institutionalization, healthcare resource utilization, and mortality risk associated with Parkinson disease psychosis: Retrospective cohort study: Parkinsonism Relat Disord, 2019; 68; 95-101
10.. Lubomski M, Rushworth RL, Tisch S, Hospitalisation and comorbidities in Parkinson’s disease: A large Australian retrospective study: J Neurol Neurosurg Psychiatry, 2015; 86(3); 324-30
11.. Aminoff MJ, Christine CW, Friedman JH, Management of the hospitalized patient with Parkinson’s disease: Current state of the field and need for guidelines: Parkinsonism Relat Disord, 2011; 17(3); 139-45
12.. Kalilani L, Asgharnejad M, Palokangas T, Durgin T, Comparing the incidence of falls/fractures in Parkinson’s disease patients in the US population: PLoS One, 2016; 11(9); e0161689
13.. Forns J, Layton JB, Bartsch J, Increased risk of falls and fractures in patients with psychosis and Parkinson disease: PLoS One, 2021; 16(1); e0246121
14.. Chou TA, Chang CY, Wang JP, Surgical outcome of upper extremity fractures in patients with Parkinson’s disease: Sci Rep, 2020; 10(1); 21016
15.. Harkin FE, Large RJ, Humeral shaft fractures: Union outcomes in a large cohort: J Shoulder Elbow Surg, 2017; 26(11); 1881-88
16.. Tukel HC, Daglioglu YK, Tatli U, Effect of botulinum toxin type A on mandibular fracture healing: An experimental study in rabbits: J Oral Maxillofac Surg, 2020; 78(12); 2281.e1-.e8
17.. Chen Y, Thalayasingam P, Botulinum toxin to control an incapacitating tic in a child with a clavicular fracture: Anaesth Intensive Care, 2010; 38(6); 1106-8
18.. Aydin A, Memisoglu K, Cengiz A, Effects of botulinum toxin A on fracture healing in rats: An experimental study: J Orthop Sci, 2012; 17(6); 796-801
19.. Canter HI, Kayikcioglu A, Aksu M, Mavili ME, Botulinum toxin in closed treatment of mandibular condylar fracture: Ann Plast Surg, 2007; 58(5); 474-78
20.. Akbay E, Cevik C, Damlar I, Altan A, Treatment of displaced mandibular condylar fracture with botulinum toxin A: Auris Nasus Larynx, 2014; 41(2); 219-21
21.. Shin SH, Kang YJ, Kim SG, The effect of botulinum toxin-A injection into the masseter muscles on prevention of plate fracture and post-operative relapse in patients receiving orthognathic surgery: Maxillofac Plast Reconstr Surg, 2018; 40(1); 36
22.. Shilt J, McHorse G, Moisiuc A, Kushare I, Chemoprotection with botulinum toxin following proximal hamstring-Ischial tuberosity avulsion fracture repair: J Clin Orthop Trauma, 2021; 12(1); 172-76
23.. White AE, Brusalis CM, Wellman DS, Taylor SA, Botulinum toxin as adjunct therapy in surgical management of a periprosthetic scapular spine fracture: A case report: Clin Shoulder Elb, 2023; 26(1); 87-92
24.. Varecka TF, Myeroff C, Distal humerus fractures in the elderly population: J Am Acad Orthop Surg, 2017; 25(10); 673-83
25.. Figueroa CA, Rosen CJ, Parkinson’s disease and osteoporosis: Basic and clinical implications: Expert Rev Endocrinol Metab, 2020; 15(3); 185-93
26.. Hausman M, Panozzo A, Treatment of distal humerus fractures in the elderly: Clin Orthop Relat Res., 2004(425); 55-63
27.. Jankovic J, Botulinum toxin: State of the art: Mov Disord, 2017; 32(8); 1131-38
28.. Kahraman A, Seyhan K, Değer Ü, Should botulinum toxin A injections be repeated in children with cerebral palsy? A systematic review: Dev Med Child Neurol, 2016; 58(9); 910-17
29.. Pirazzini M, Rossetto O, Eleopra R, Montecucco C, Botulinum neurotoxins: Biology, pharmacology, and toxicology: Pharmacol Rev, 2017; 69(2); 200-35
30.. Hao Y, Ma Y, Wang X, Short-term muscle atrophy caused by botulinum toxin-A local injection impairs fracture healing in the rat femur: J Orthop Res, 2012; 30(4); 574-80
Figures
In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250