22 November 2023: Articles 
A 21-Year-Old Woman with Sickle Cell Disease and Vaso-Occlusive Pain Associated with Using an Electronic Nicotine Dispensing System (E-Cigarette or Vape) – a Case Report
Rare disease, Adverse events of drug therapy, Clinical situation which can not be reproduced for ethical reasons
Ganga GirishDOI: 10.12659/AJCR.941268
Am J Case Rep 2023; 24:e941268
Abstract
BACKGROUND: Sickle cell disease is an inherited blood disorder that leads to multisystem complications. The heterogeneous course of sickle cell disease is due to both genetic modifiers and environmental factors. Cigarette smoking is a strong risk factor for sickle cell complications and even secondhand exposure to tobacco smoke can be detrimental for individuals with sickle cell disease. However, no prior reports have associated e-cigarettes and sickle cell vaso-occlusive pain.
CASE REPORT: A 21 year old woman presented with sickle cell disease SS complicated by frequent pain, multiple acute chest syndrome episodes, sickle cell nephropathy, and avascular necrosis of the left hip, plus mild intermittent asthma. She developed pain in the ribs and back after her first use of e-cigarettes. After 4 days of home pain management, she came to the Emergency Department. She was mildly hypoxic and received supplemental oxygen. Chest radiograph did not show airspace consolidation, and the sites of pain were consistent with her prior pain episodes, so the diagnosis was sickle cell vaso-occlusive pain. Her hemoglobin was more than 2 g/dL below baseline and she received a red blood cell transfusion on hospital day 2. Overall, this was among her more severe pain episodes.
CONCLUSIONS: The rising popularity of e-cigarettes, also known as vapes or Electronic Nicotine Delivery Systems (ENDS), is partly due to the misconception that they are safer than traditional cigarettes. Although firm conclusions will depend on studies designed to provide rigorous evidence, this case suggests that the acute adverse effects of ENDS might trigger complications of sickle cell disease, especially with asthma as a comorbidity.
Keywords: Anemia, Sickle Cell, Vaping, young adult, Female, case reports
Background
Sickle cell disease (SCD) is a complex autosomal recessive blood disease [1,2]. To the authors’ knowledge, no prior reports have associated e-cigarettes and vaso-occlusive pain in SCD.
Sickle hemoglobin (HbS) results from a point mutation in the beta chain of hemoglobin that replaces glutamate with valine [1–3]. SCD (Table 1) encompasses several genotypes: individuals with 2 copies of the HbS mutation (SCD-SS, also known as sickle cell anemia), individuals with 1 copy of HbS and another gene that produces a different abnormal hemoglobin, such as hemoglobin C (SCD-SC) or D (SCD-SD), and individuals with 1 copy of HbS and 1 gene that expresses quantitatively less hemoglobin (beta-zero thalassemia or beta-plus thalassemia). Of these different genotypes of SCD, the most common are SCD-SS & SCD-SC in the United States [3].
Under conditions such as hypoxia, stress, serious illness, or cold environmental conditions, the mutated HbS molecule can form rigid, 14-stranded polymers within the erythrocytes when deoxygenated, distorting the red blood cell into an elongated sickle shape (Figure 1) [1–4]. HbS is unstable, leading to spontaneous denaturation, oxidant damage, and precipitation onto the red blood cell (RBC) membrane. Another abnormal property of sickle cells is increased adhesion molecules that bind to the endothelial walls. Finally, sickle cells have a high tendency to hemolyze, releasing components that incite an inflammatory response, which also leads to vaso-occlusion [2,4].
SCD can damage multiple organ systems with a complex pathophysiology of ischemia, inflammation, vasculopathy, and oxidant stress, including: acute chest syndrome, stroke, nephropathy, retinopathy, avascular necrosis, priapism, and leg ulcers [1–4]. However, the hallmark of SCD is vaso-occlusive crisis (VOC). Blockage of the blood flow leads to severe, unrelenting bone pain arising from ischemia-reperfusion injury and inflammation. This acute, painful vaso-occlusion can be amplified by a complex pathophysiology involving neuropathic and central pain pathways along with local nociceptive pain. Management of VOC mainly emphasizes symptomatic treatment of pain with analgesics [1,2].
Strategies to prevent VOC begin with lifestyle choices and include modern disease-modifying therapies. Progress in medications for SCD has been accelerating and several excellent reviews discuss details of the treatments and their mechanisms [2,5,6] but the medications are briefly mentioned here. Chronic monthly blood transfusions were the first successful treatments to significantly reduce the complications of SCD. The first medication shown to reduce the severity of SCD was hydroxyurea, approved by the United States Food and Drug Administration (FDA) in 1998. The FDA approved glutamine for SCD in 2017, and then approved both voxelotor and crizanlizumab in 2019. Voxelotor binds covalently to HbS and keeps it in the oxy-conformation, blocking HbS polymerization, sickle deformation, and hemolysis [2,6]. Meanwhile, hematopoietic stem cell transplant from a sibling donor has become established as a curative therapy, with over 2000 successful transplants worldwide [2]. Transplants from alternative donors and gene therapy have made great strides in the past few years [2]. Adoption of all these therapies is heterogeneous, but multiple clinical trials have demonstrated that hydroxyurea can be successfully combined with other therapies [2].
To the authors’ knowledge, no prior reports have associated e-cigarettes and vaso-occlusive pain in SCD. Smoking cigarettes is a strong risk factor for sickle cell complications [7,8] and the adverse impact of secondhand exposure to tobacco smoke on SCD has been an active research topic [9,10]. The present report is of a 21-year-old woman with asthma and SCD, treated with voxelotor, who presented with vaso-occlusive pain after using an Electronic Nicotine Delivery System (ENDS), also known as an e-cigarette or vape.
Case Report
PATIENT INFORMATION:
A 21 year old woman presented with SCD-SS complicated by frequent pain, 6 acute chest syndrome episodes, sickle cell nephropathy, and avascular necrosis of the left hip, plus mild intermittent asthma. Other history included streptococcal bacteremia and pneumonia at 7 years of age and hemolytic transfusion reaction with alloimmunization at 16 years of age. Her sickle cell vaso-occlusive pain had a history of being triggered by infection, dehydration, temperature extremes, exertion, or emotional stress. She had been on voxelotor 1500 mg daily for 4 months and reported missing about 1 dose per week. Voxelotor was started after 3 years of hydroxyurea therapy was stopped for reticulated rash and lack of benefit. She used an albuterol inhaler about once a week upon moderate physical exertion. She never smoked cigarettes.
CLINICAL FINDINGS:
She had severe rib and back pain that was consistent with the pattern of several previous sickle cell vaso-occlusive pain episodes. The pain had been worsening for 4 days and she had minimal relief from home pain management with lidocaine transdermal patches, menthol/methyl salicylate cream, extended-release morphine 15 mg, and hydrocodone-acetaminophen 10–325 mg. Her mother reported that her pain crisis was triggered by the use of an e-cigarette. The patient confirmed that she and a friend were vaping for the first time and that her pain started afterward. She showed us the e-cigarette (brand name Vaporesso XROS) in her purse and gave it to us, stating that she did not want to use it any more.
DIAGNOSTIC ASSESSMENT:
The patient described the pain as a 9 on a scale of 10 and consistent with her prior vaso-occlusive episodes. Her oxygen saturation was 92%. Her hemogram was significant for leukocytosis to 25.5. Her hemoglobin and reticulocyte count, at 8.5 and 12.4 respectively, were both around her baseline. Chest radiograph (Figure 2) did not show airspace consolidation, and thus she did not meet the definition for sickle acute chest syndrome; namely, a new infiltrate on chest imaging plus any 2 of the following: pleuritic chest pain, hypoxemia, tachypnea, or fever [2].
THERAPEUTIC INTERVENTIONS:
In the Emergency Department, she was given 3 intravenous doses of morphine 10 mg spaced 1 hour apart for pain control and supplemental oxygen 2 L/min by nasal cannula. She was then admitted to the hospital for further management of pain. On her first day of hospitalization, she was started on a pain control regimen of intravenous morphine 6 mg every 4 hours, hydrocodone-acetaminophen 10–325 mg every 6 hours, lido-caine transdermal patches, and analgesic balm. On the second day of hospitalization, her hemoglobin dropped to 5.9 g/dL.
FOLLOWUP AND OUTCOMES:
She received RBC transfusion with prednisone due to a history of delayed transfusion reaction, with tapered doses of the prednisone over the next 7 days. She reported improvement in pain, allowing for a gradual taper of her intravenous morphine and transition to morphine-extended-release p.o. 30 mg on the third day, and was weaned off supplemental oxygen. However, on day 4, she witnessed the emergency resuscitation of another patient and suffered emotional distress plus suffered cold exposure when her bed was moved to the hallway and then to another room. This unfortunate upsetting situation led to another crisis episode with worsened pain requiring switching back to morphine IV 10 mg every 3 hours. Over the next several days, she gradually reported improvement again and the morphine was tapered again. No signs of hemolytic transfusion reaction appeared. Finally, she was discharged home on hospital day 7 with morphine p.o. 30 mg twice a day and hydrocodone-acetaminophen 10–325 mg as needed. Overall, this was among her more severe pain episodes.
Discussion
ENDS have not been reported to cause pain, but the mechanisms of adverse effects of ENDS do appear to overlap with the pathophysiology of sickle cell vaso-occlusive pain, with further amplification of inflammatory effects of ENDS in a patient with asthma such as the patient in this case report.
ENDS use a battery-powered heating element to aerosolize a nicotine solution that is inhaled into the lungs [11,12]. The vaping liquid/e-liquid/e-juice also includes compounds like propylene glycol and/or vegetable glycerol, water, flavoring compounds like diacetyl, and flavor enhancers. The rise in popularity of vaping products is due, in part, to the mistaken belief that they are a safer alternative to traditional cigarettes. Additionally, the pleasant smells produced by the flavoring compounds in vaping liquids can make the emissions seem benign. Although advertised as safer than combustible cigarettes, ENDS have potential acute and chronic adverse effects that could amplify the complications of asthma and SCD. Acute airway complications include bronchoconstriction, transient hypoxia, lung inflammation, and throat irritation from propylene glycol and formaldehyde [13–16]. Chronic exposure to ENDS has potential adverse effects beyond the airways to include cardiovascular and neurologic dysfunction, plus cancer risk, through pathophysiologic mechanisms that include inflammation and oxidant stress [11,12].
The only other case report of pain as an adverse effect of ENDS was priapism in an individual without SCD [17]. Stuttering priapism (painful penile erection in an intermittent pattern) started approximately 1 week after a 31-year-old man switched from cigarettes to using ENDS. The priapism completely resolved after he stopped. That case report discussed the pathophysiology of priapism and how it is associated with loss of nitric oxide vasoregulation, and speculated that the ENDS might be depleting nitric oxide and thereby causing priapism [17]. Priapism is a common complication of SCD-SS, and a large body of evidence links nitric oxide depletion to sickle cell priapism [2,18].
Sickle cell vaso-occlusive pain in other locations of the body has multifactorial pathophysiology. However, nitric oxide consumption and reduced nitric oxide production are well-recognized components of SCD pathophysiology, especially linked to hemolysis and oxidant stress [4,19]. In addition, asthma and sickle cell pathophysiology appear to overlap in heightened inflammatory responses [20,21]. Thus, oxidant stress and nitric oxide depletion as acute adverse effects of ENDS overlap with the pathophysiologic processes of sickle vaso-occlusion, with potential further amplification of inflammatory effects of ENDS in a patient with asthma such as the patient in this case report.
Conclusions
In this patient with SCD-SS and asthma, her first use of ENDS was associated with onset of sickle cell vaso-occlusive pain. The potential for ENDS to cause acute lung inflammation and nitric oxide dysregulation overlaps with the pathophysiology of SCD, making it plausible that ENDS triggered a vaso-occlusive pain episode that was severe enough to need hospitalization. Although this case report is certainly not rigorous evidence, we hypothesize that ENDS could hold heightened risks for individuals with SCD and asthma. Further study is needed.
Figures
References:
1.. Kimrey S, Saving KL, Sickle cell disease: A primer for primary care providers: Pediatr Ann, 2020; 49(1); e43-e49
2.. Kavanagh PL, Fasipe TA, Wun T, Sickle cell disease: A review: JAMA, 2022; 328(1); 57-68
3.. , Sickle cell disease July 6, 2023 Accessed September 16, 2023. https://www.cdc.gov/ncbddd/sicklecell/facts.html
4.. Sundd P, Gladwin MT, Novelli EM, Pathophysiology of sickle cell disease: Annu Rev Pathol, 2019; 14; 263-92
5.. Osunkwo I, Manwani D, Kanter J, Current and novel therapies for the prevention of vaso-occlusive crisis in sickle cell disease: Ther Adv Hematol, 2020; 11; 2040620720955000
6.. Inusa BPD, Mnika K, Babiker S, An expert review of voxelotor for the treatment of hemolytic anemia in patients with sickle cell disease: ‘Bridging the gap between laboratory data and patient related outcomes’: Expert Rev Hematol, 2023; 16(8); 585-91
7.. Young RC, Rachal RE, Hackney RL, Smoking is a factor in causing acute chest syndrome in sickle cell anemia: J Natl Med Assoc, 1992; 84(3); 267-71
8.. Nawaiseh M, Roto A, Nawaiseh Y, Risk factors associated with sickle cell retinopathy: Findings from the Cooperative Study of Sickle Cell Disease: Int J Retina Vitreous, 2022; 8(1); 68
9.. Sadreameli SC, Eakin MN, Robinson KT, Secondhand smoke is associated with more frequent hospitalizations in children with sickle cell disease: Am J Hematol, 2016; 91(3); 313-17
10.. Tackett AP, Leavens ELS, Wiedenmann A, Preliminary exploration of secondhand smoke exposure in youth with sickle cell disease: Biochemical verification, pulmonary functioning, and health care utilization: Psychol Health Med, 2019; 24(1); 35-42
11.. Rose JJ, Krishnan-Sarin S, Exil VJ, Cardiopulmonary impact of electronic cigarettes and vaping products: A Scientific Statement From the American Heart Association: Circulation, 2023; 148(8); 703-28
12.. Esteban-Lopez M, Perry MD, Garbinski LD, Health effects and known pathology associated with the use of E-cigarettes: Toxicol Rep, 2022; 9; 1357-68
13.. Chaumont M, van de Borne P, Bernard A, Fourth generation e-cigarette vaping induces transient lung inflammation and gas exchange disturbances: Results from two randomized clinical trials: Am J Physiol Lung Cell Mol Physiol, 2019; 316(5); L705-L19
14.. Shinbashi M, Rubin BK, Electronic cigarettes and e-cigarette/vaping product use associated lung injury (EVALI): Paediatr Respir Rev, 2020; 36; 87-91
15.. Nicol J, Fraser R, Walker L, Comprehensive chemical characterization of the aerosol emissions of a vaping product based on a new technology: Chem Res Toxicol, 2020; 33(3); 789-99
16.. Bonner E, Chang Y, Christie E, The chemistry and toxicology of vaping: Pharmacol Ther, 2021; 225; 107837
17.. Alzahrani AM, Basalelah JH, Alarifi MS, Alsuhaibani SS, Electronic cigarettes as a cause of stuttering priapism: A case report: Am J Case Rep, 2021; 22; e935716
18.. Joice GA, Liu JL, Burnett AL, Medical treatment of recurrent ischaemic priapism: A review of current molecular therapeutics and a new clinical management paradigm: BJU Int, 2021; 127(5); 498-506
19.. Kato GJ, Steinberg MH, Gladwin MT, Intravascular hemolysis and the patho-physiology of sickle cell disease: J Clin Invest, 2017; 127(3); 750-60
20.. Samarasinghe AE, Rosch JW, Convergence of inflammatory pathways in allergic asthma and sickle cell disease: Front Immunol, 2020; 10; 3058
21.. Field JJ, DeBaun MR, Asthma and sickle cell disease: Two distinct diseases or part of the same process?: Hematology Am Soc Hematol Educ Program, 2009; 45-53
Figures
Tables
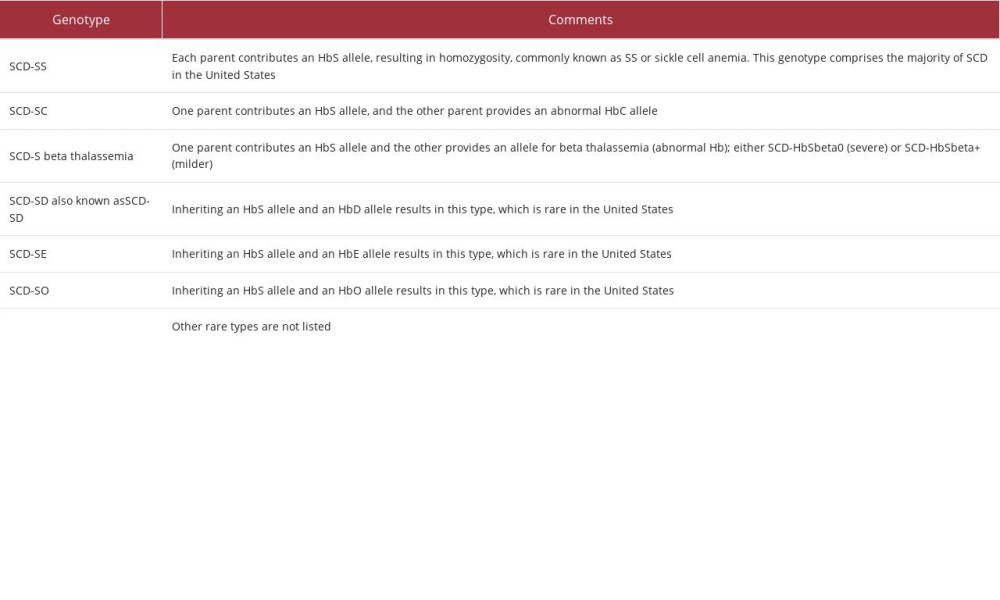 Table 1.. Sickle cell disease (SCD) genotypes. All genotypes can have manifestations of sickle disease: rigid deformation of red blood cells, hemolytic anemia, ischemic organ damage, and vaso-occlusive pain [1–3]. Very rare genotypes are not listed.
Table 1.. Sickle cell disease (SCD) genotypes. All genotypes can have manifestations of sickle disease: rigid deformation of red blood cells, hemolytic anemia, ischemic organ damage, and vaso-occlusive pain [1–3]. Very rare genotypes are not listed.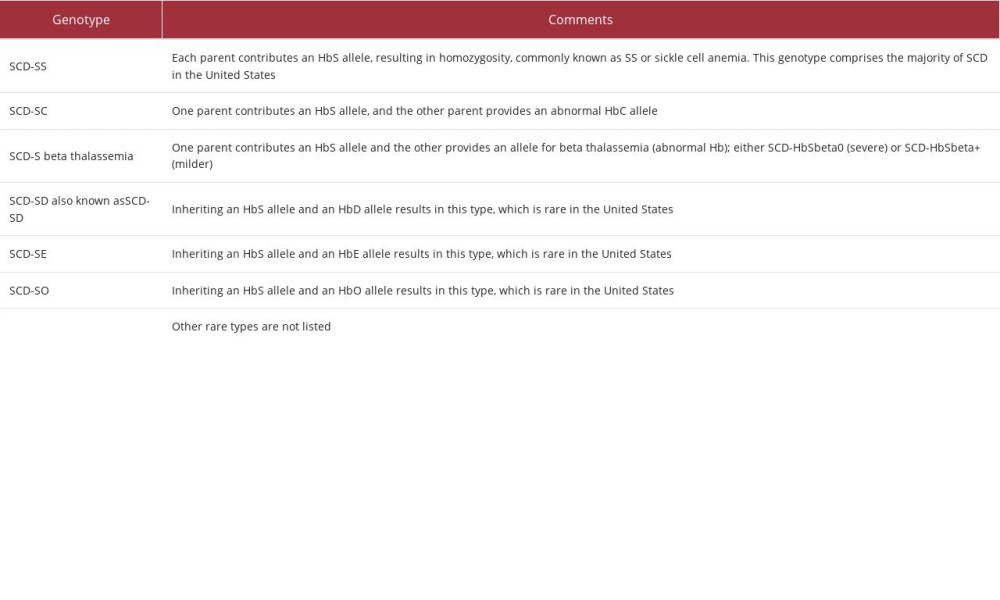 Table 1.. Sickle cell disease (SCD) genotypes. All genotypes can have manifestations of sickle disease: rigid deformation of red blood cells, hemolytic anemia, ischemic organ damage, and vaso-occlusive pain [1–3]. Very rare genotypes are not listed.
Table 1.. Sickle cell disease (SCD) genotypes. All genotypes can have manifestations of sickle disease: rigid deformation of red blood cells, hemolytic anemia, ischemic organ damage, and vaso-occlusive pain [1–3]. Very rare genotypes are not listed. In Press
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








