23 October 2023: Articles 
An Elusive Diagnosis: Diffuse Large B-Cell Lymphoma Masquerading as Acute Liver Failure with Persistent Lactic Acidosis
Challenging differential diagnosis, Rare disease
Prabasha WeeraddanaDOI: 10.12659/AJCR.941270
Am J Case Rep 2023; 24:e941270
Abstract
BACKGROUND: Acute liver failure (ALF) associated with malignant lymphoma is a rare condition with non-specific clinical and radiological features. Here, we describe an unusual case of ALF due to DLBCL with an image negative on presentation posing diagnostic difficulty.
CASE REPORT: A 74-year-old man was admitted to our hospital with abdominal pain. Radiological and laboratory investigations revealed lymphadenopathy with mildly elevated transaminitis and alkaline phosphates levels. A right upper-quadrant ultrasound showed heterogeneous hepatic parenchyma. Eight days later, he had worsening abdominal pain. He was found to have altered mental status and asterixis. His liver function was worsened with ALT 101, AST 328, lactic acid 4.2, total bilirubin 2.5, INR 6.35, and ammonia level 117 µmol/L. He continued to deteriorate with worsening lactic acidosis, coagulopathy, severe anemia, elevated liver enzymes, and thrombocytopenia. Unfortunately, the patient died of multi-organ failure on the 14th day of hospitalization. The autopsy findings revealed DLBCL involving multiple organs, including the liver, lung, bone marrow, and multiple lymph nodes. Despite an extensive diagnostic workup, an underlying diagnosis was unable to be established antemortem.
CONCLUSIONS: We describe a case of ALF linked to DLBCL discovered at autopsy. The non-specific clinical and radiological features of this condition make diagnosis challenging, and the prognosis is often poor. Further research and awareness are needed to improve the early detection and management of ALF associated with malignant lymphoma. By expanding the literature on this topic, we aim to improve outcomes and optimize patient care in similar clinical scenarios.
Keywords: Autopsy, Liver Failure, Acute, Male, Humans, Aged, Acidosis, Lactic, Lymphoma, Large B-Cell, Diffuse, Abdominal Pain
Background
Acute liver failure refers to the development of severe acute liver injury with impaired synthetic function (INR of ≥1.5) and altered mental status in a patient without preexisting cirrhosis and with an illness of <26 weeks duration [1]. ALF due to malignant infiltration is quite uncommon compared to much more common causes that include adverse drug reactions (acetaminophen toxicity) and viral hepatitis [2]. Here, we present a case of ALF associated with diffuse large B-cell lymphoma discovered at autopsy.
Case Report
A 74-year-old man with a past medical history of obstructive sleep apnea (OSA), interstitial lung disease (ILD), morbid obesity, hypertension, atrial fibrillation, and diabetes mellitus presented to the hospital with a chief concern of epigastric abdominal pain radiating to his chest associated with progressive abdominal distension, poor appetite, nausea, belching, and constipation. His cardiac workup was negative for acute coronary syndrome. He underwent computed tomography (CT) of the abdomen and pelvis, which showed moderate colonic stool consistent with constipation, as well as enlarged pelvic, mediastinal, and retroperitoneal lymph nodes (a mild increase in size since the last imaging in 2018). In 2018, he underwent bronchoscopy with fine-needle aspiration of a level 7 lymph node with flow cytometry analysis, which had not revealed a specific pathology. Laboratory examination results were un-remarkable, and the patient was discharged with a plan for an aggressive bowel regimen at home. He presented to the Emergency Department again the next day with no improvement in pain and worsening abdominal distension. On presentation, the patient was using his baseline oxygen via nasal cannula, and his vital signs were within normal limits. On examination, the abdomen was soft, mildly distended, and non-tender to palpation, without rebound tenderness or guarding. The patient’s admission laboratory values are shown in Table 1. A repeat CT of the chest (Figure 1), abdomen, and pelvis again revealed chest, abdominal, and pelvic adenopathy, and aortoiliac atherosclerotic disease. A right upper-quadrant ultra-sound showed heterogeneous and coarsened echotexture of the hepatic parenchyma, without evidence of biliary tree or gallbladder disease. Based on the clinical presentation and the patient’s history of paroxysmal atrial fibrillation, there was a concern for acute mesenteric ischemia. A CT angiography of the abdomen was performed and showed extensive atherosclerosis of the superior mesenteric artery with at least moderate stenosis at the ostium. Subsequent endoscopy revealed a non-obstructing Schatzki ring and gastric ulcer with oozing hemorrhage, which was treated with bipolar cautery. His serum immunofixation (IFE) showed 0.2 g/dL of M spike in the background of polyclonal gammopathy, with IFE identifying IgM kappa. Quantitative IgM was found to be mildly elevated at 233 mg/dL. The free light chain ratio was normal. Flow cytometry of peripheral blood showed no evidence of increased blast proliferation or lymphoproliferative disease. The patient declined to undergo a bone marrow biopsy. Eight days later, he had worsening abdominal pain, and was found to have altered mental status and asterixis. He was afebrile, and his vitals were within normal range, with oxygen saturation at 94%. Labs showed a white blood cell count of 16.4×109/L, platelets of 89×109/L, ALT 101 U/L, AST 328 U/L, lactic acid 4.2 mmol/L, total bilirubin 2.5 mg/dL, direct bilirubin 1.9 mg/dL, INR 6.35, and ammonia level 117 µmol/L. Repeat CT of the abdomen and pelvis showed no acute findings. Given the worsening abdominal pain and encephalopathy, with lab work showing elevated transaminases, lactic acidosis, and coagulopathy, the patient was transferred to the progressive care unit (PCU) for acute liver failure. He was started on an intravenous (IV) N-acetylcysteine drip, lactulose, and 10 mg IV vitamin K. Given his acute encephalopathy, a CT head was performed, which ruled out any acute abnormalities. EEG was abnormal due to the presence of diffuse slowing. Serology was negative for HAV, HBV, HCV, HIV, EBV, and CMV. A tick panel was negative. Anti-smooth muscle antibodies were negative. Unfortunately, the patient continued to worsen clinically, and his respiratory status began to decompensate. His chest radiography (CXR) showed bilateral ground-glass opacities concerning for pneumonia. He was subsequently started on broad-spectrum antibiotics. The next day, he was noted to be more lethargic and tachypneic. ABG was obtained, which showed pH 7.46, pCO2 34 mmHg, and HCO3 24 mEq/L. He was placed on bilevel-positive airway pressure (BiPAP). On the next day, he was admitted to the intensive care unit (ICU) after failing BiPAP for respiratory failure in the PCU. He was unresponsive, comatose, and hypotensive, with worsening markers of what appeared to be septic shock. Blood workup showed increasing lactic acidosis at 7.3 mmol/L, increasing total bilirubin at 7.9 mg/dL, direct bilirubin at 5.3 mg/dL, ALT 174 U/L, AST 396 U/L, reduced hemoglobin at 6.6 g/dL, critical thrombocytopenia to 29×109/L, and prolonged INR at 7.04. The decision was made to intubate the patient. The diagnostic workup for infection revealed gram-negative bacteremia and evidence of septic shock, for which he had been started on IV fluids and vasopressors. Unfortunately, the patient’s ICU stay was complicated by ventricular tachycardia. He was defibrillated twice and returned to atrial fibrillation with a rapid ventricular response. He later developed acute respiratory distress syndrome (ARDS) and continued to deteriorate. Given the overall worsening prognosis, the patient’s family decided to initiate comfort care and palliative extubation. The patient died the next morning on hospital day 14.
Autopsy findings revealed diffuse large B-cell lymphoma involving multiple organs, including the liver, lung, bone marrow, and multiple lymph nodes. On gross examination, there was extensive lymphadenopathy involving the right cervical, peri-bronchial, subcarinal, and pelvic lymph nodes. A large mass (9×6.5×4 cm) comprised of matted lymph nodes was present in the right lung hilum. The liver was enlarged, which on sectioning revealed multiple ill-defined pale-yellow nodules. On histopathologic examination, the enlarged lymph nodes showed infiltration of medium-to-large atypical lymphoid cells with vesicular chromatin, variably prominent nucleoli, and a scant-to-moderate amount of cytoplasm. By immunohistochemical staining, the atypical cells were diffusely strongly positive for CD20, CD10, and BCL-2 and negative for cyclin D1, CD5, CD138, MUM1, CD21, CD3, and BCL6. The immunophenotypic findings were consistent with diffuse large B-cell lymphoma, germinal center B-cell subtype (Figure 2). Sections of the liver showed areas of necrosis as well as nodular and diffuse infiltrate of atypical medium-to-large CD20+ cells, consistent with involvement by diffuse large B-cell lymphoma (Figure 3). Bone marrow sections showed greater than 90% involvement by diffuse large B-cell lymphoma (Figure 4).
Discussion
This case demonstrates ALF associated with diffuse large B-cell lymphoma (DLBCL). Acute liver failure is characterized by an acute liver injury (transaminitis, lactic acidosis, and jaundice), hepatic encephalopathy, and an abnormal coagulation profile (INR >1.5), all of which were observed in this patient [1]. It is reported to last for 26 weeks. In Europe and the US, the most prevalent causes of ALF are acetaminophen overdose, unusual medication reactions, and viral hepatitis [2]. DLBCL is a form of non-Hodgkin lymphoma that develops in either lymph nodes or in extra-nodal sites that can essentially be any organ of the body (eg, gastrointestinal tract, liver, skin, breast, prostate). It can remain localized or spread throughout the body.
According to Rich et al, only 10% of patients with ALF had an associated malignancy. Of these patients, 33% reported lymphomas and leukemias, whereas the contribution of other malignancies was breast cancer (30%) and colon cancer (7%) [4]. Of all lymphomas that can infiltrate the liver, diffuse large B-cell lymphoma is the commonest with this association [5]. Non-germinal center type DLBCL is more commonly involved with liver involvement [6]; however, our patient had immunohisto-chemical features of a germinal center type DLBCL. The typical clinical manifestations of ALF caused by metastatic infiltration involve jaundice, hepatic encephalopathy, and hepatomegaly. Radiologic, laboratory, and clinical findings are often non-specific and inconclusive. In most cases, the diagnosis of ALF due to metastatic infiltration is made postmortem [7,8]. While a premortem diagnosis is possible through liver or bone marrow biopsies, only 25% of cases are identified prior to death, according to a recent literature review [9]. Treatment options for ALF caused by a neoplastic invasion are limited, as starting chemotherapy in the setting of ALF is challenging. ALF resulting from a neoplastic invasion generally carries a worse prognosis, with death occurring within 3 days to 6 months of presentation [7]. Liver transplantation is not considered suitable for cases of liver metastasis. However, there have been a few clinical cases where liver transplantation and adjuvant chemotherapy were successfully performed in patients with unrecognized metastatic disease. Additionally, rare cases of ALF reversal from metastatic breast cancer have been reported following chemotherapy, resulting in longer survival of up to 9 months [4,10].
ALF due to DLBCL is uncommon, and to date only 17 cases have been reported. In those cases, the prognosis has been generally poor, with high rates of in-hospital mortality. Three cases were diagnosed at autopsy [11]. A summary of previously documented cases of acute liver failure due to infiltration of the liver by non-Hodgkin lymphoma is shown in Table 2.
Our patient met all the criteria for the diagnosis of acute liver failure; however, the etiology of this was not established prior to death. A possible hematologic malignancy was considered based on persistent lymphadenopathy, but the patient refused to undergo a bone marrow biopsy, and this prevented the early diagnosis and start of treatment. In a study by Rich et al, liver biopsy was found to be a hallmark in the early diagnosis of such patients [4], but bone marrow biopsy and gastric biopsy can also help with the diagnosis. Early diagnosis of DLBCL provides the chance for proper treatment of patients with chemotherapy, and this has proved to decrease the mortality rate [11]. However, liver biopsy should be carefully considered in patients with ALF due to the risk of complications that can be exacerbated by coagulopathy and thrombocytopenia.
The prognosis of malignancy-induced ALF usually is worse than the prognosis of ALF secondary to other causes [12]. One of the largest single-center studies reported a 0.44% incidence rate of ALF due to malignant infiltration by hematological malignancies, with a mortality rate of 94% [13]. Lactic acidosis is a common feature of acute liver failure. As with our patient, other authors reported significant lactic acidosis in their patients. In fact, it was one of the first features in the case written by Gkoufa et al [14] before a histological diagnosis of DLBCL was made based on liver and bone biopsy, and the only unique feature was that the liver and bone marrow were involved by lymphoma. Various mechanisms have been explained for the occurrence of lactic acidosis in patients with acute liver failure, including impaired metabolism and enhanced aerobic glycolytic activity in tumor cells because of the over-expression of certain glycolytic enzymes [15].
The radiologic features of acute liver failure associated with malignant infiltration remain unclear [11]. Ultrasound findings in our patient revealed the non-specific heterogeneous and coarse architecture of the hepatic parenchyma, without evidence of biliary tree or gall bladder disease. This is similar to the findings described by other authors, where CT scans performed on the patients showed no distinct nodules or masses in the liver [6,11,14]. While it seems that radiologic studies might have poor ability to detect liver masses caused by infiltration by malignant lymphomas, it is plausible that the only way to increase the detection of these cases is by attempting a liver biopsy [4].
DLBCLs infiltrating the liver are usually present late during the clinical course. It is usually difficult to treat these patients, even if it is promptly diagnosed, as multi-organ dysfunction usually has already occurred. In addition, even if a prompt diagnosis is made, treatment is still a challenge, as many of the chemotherapeutic agents required for treatment are metabolized by the liver, and their administration can worsen the clinical outcome [16]. While the mortality rate of acute liver failure due to infiltration by DLBCLs is high, some authors have described cases of patients surviving as a result of prompt treatment [13,16,17].
Various mechanisms have been suggested as the cause for acute liver failure in patients with infiltration of the liver by DLBCLs, including localized or diffuse parenchymal necrosis secondary to malignant infiltration, tumor infiltration of the biliary tree, and tumor infiltration of the hepatic vasculature [18,19]. In our patient, it seems likely that a combination of hepatocyte damage and biliary obstruction from biliary tree infiltration occurred, as the transaminases and alkaline phosphatase were all elevated.
In our patient, autopsy findings were consistent with DLBCL. His ALF was most likely secondary to liver infiltration by a hematological malignancy, given the initial mild elevation of ALT/ AST and alkaline phosphatase with a normal bilirubin profile. The cause of death in this 74-year-old man was primarily acute liver failure secondary to diffuse large B-cell lymphoma infiltrating the liver, later complicated by multi-organ failure. As a result, our study is a useful addition to the literature on ALF.
Conclusions
ALF secondary to DLBCL can be a rare presentation of this hematological malignancy associated with a poor prognosis. This critical condition could be suspected in cases of persistent lactic acidosis, worsening coagulopathy, and increasing ammonia levels in the context of diffuse lymphadenopathy and the absence of other common causes of ALF.
Figures
References:
1.. Polson J, Lee WM, AASLD position paper: The management of acute liver failure: Hepatology, 2005; 41(5); 1179-97
2.. Ostapowicz G, Fontana RJ, Schiødt FV, Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States: Ann Intern Med, 2002; 137(12); 947-54
3.. Mochida S, Takikawa Y, Nakayama N, Diagnostic criteria of acute liver failure: A report by the Intractable Hepato-Biliary Diseases Study Group of Japan: Hepatol Res, 2011; 41(9); 805-12
4.. Rich NE, Sanders C, Hughes RS, Malignant infiltration of the liver presenting as acute liver failure: Clin Gastroenterol Hepatol, 2015; 13(5); 1025-28
5.. Loddenkemper C, Longerich T, Hummel M, Frequency and diagnostic patterns of lymphomas in liver biopsies with respect to the WHO classification: Virchows Arch, 2007; 450(5); 493-502
6.. Grille S, Boada M, Bove V, Diffuse large B cell lymphoma presenting with acute liver failure: A case report. Case reports in Clin: Pathology, 2015; 2(3); 53-58
7.. Goswani R, Babich M, Farah KF, Occult breast malignancy masquerading as acute hepatic failure: Gastroenterol Hepatol, 2011; 7; 62-64
8.. Sass DA, Clark K, Grzybicki D, Diffuse desmoplastic metastatic breast cancer simulating cirrhosis with severe portal hypertension: A case of “pseudocirrhosis”: Dig Dis Sci, 2007; 52; 749-52
9.. Mogrovejo E, Manickam P, Amin M, Characterization of the syndrome of acute liver caused by metastases from breast carcinoma: Dig Dis Sci, 2014; 59; 724-36
10.. Giuliani J, Bonetti A, Acute liver failure caused by metastatic breast cancer: Can we expect some results from chemotherapy?: Dig Dis Sci, 2015; 60(8); 2541-43
11.. Kubo K, Kimura N, Mabe K, Acute liver failure associated with diffuse large B-cell lymphoma: An autopsy case report: Clin J Gastroenterol, 2022; 13(6); 1213-18
12.. Rao RL, Hornstein N, Britten K, Successful treatment of diffuse large B cell lymphoma presenting as acute liver failure: Ann Hematol Oncol, 2021; 8(8); 1359
13.. Rowbothan D, Wendon J, Williams R, Acute liver failure secondary to hepatic infiltration. A single center experience of 18 cases: Gut, 1998; 42; 576-80
14.. Gkoufa A, Georgakopoulou V, Lakiotaki E, Cholongitas E, An unusual presentation of diffuse large B-cell lymphoma: Cureus, 2022; 14(1); e20927
15.. Liberti MV, Locasale JW, The Warburg effect: How does it benefit cancer cells?: Trends Biochem Sci, 2016; 41; 211-18
16.. Shibata J, Kurahashi S, Naibo T, Sugiura I, Diffuse large B cell lymphoma primarily presenting as acute liver failure in a surviving patient: J Community Hosp Intern Med Perspect, 2019; 9(2); 135-39
17.. Kapuria D, Strasse K, Qasem A, Diffuse large B-cell lymphoma causing acute liver failure: A rare case of survival: BMJ Case Rep, 2015; 2015; bcr2015209328
18.. Zafrani ES, Leclercq B, Vernant JP, Massive blastic infiltration of the liver; A cause of fulminant hepatic failure: Hepatology, 1983; 3; 428-32
19.. Myszor MF, Record CO, Primary and secondary malignant disease of the liver and fulminant hepatic failure: J Clin Gastroenterol, 1990; 12; 441-46
Figures
Tables
 Table 1.. Day-to-day laboratory findings (Day 0 is the day of admission).
Table 1.. Day-to-day laboratory findings (Day 0 is the day of admission).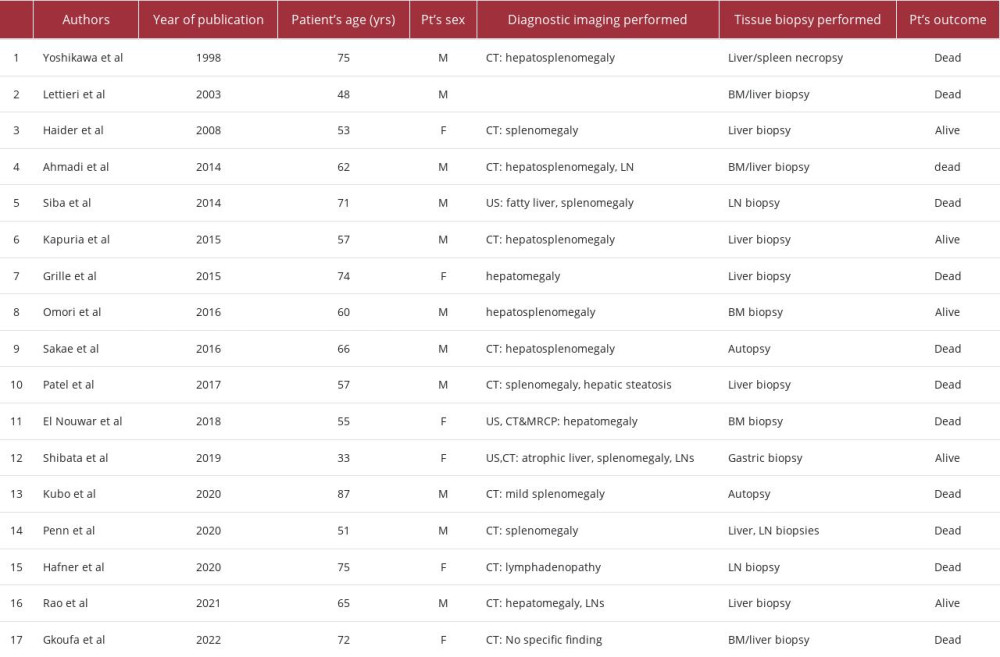 Table 2.. Cases reported to date of acute liver failure secondary to infiltration of the liver by non-Hodgkin lymphoma.
Table 2.. Cases reported to date of acute liver failure secondary to infiltration of the liver by non-Hodgkin lymphoma. Table 1.. Day-to-day laboratory findings (Day 0 is the day of admission).
Table 1.. Day-to-day laboratory findings (Day 0 is the day of admission).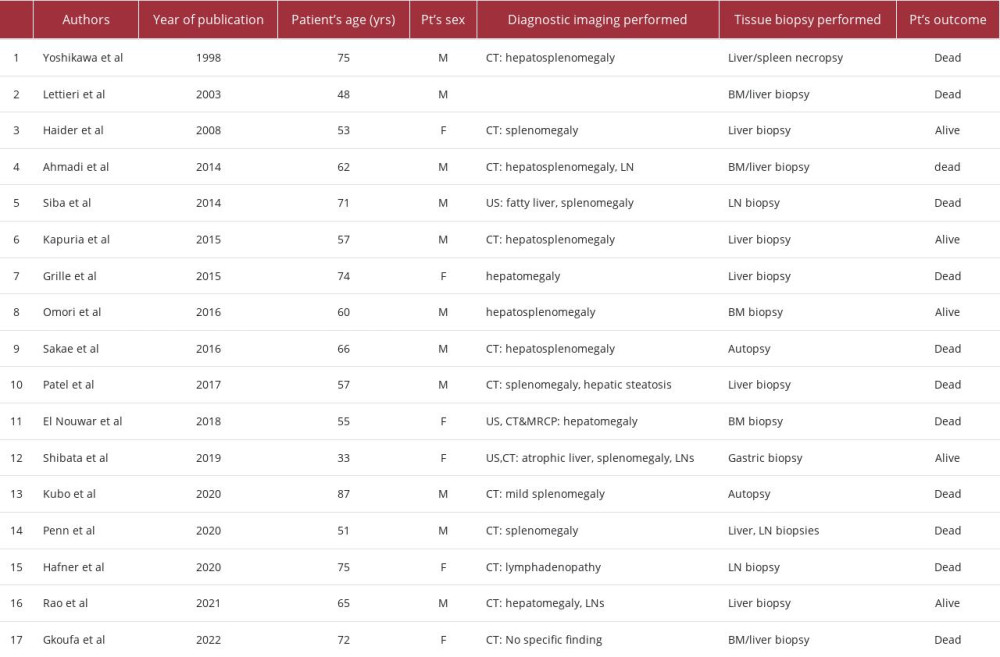 Table 2.. Cases reported to date of acute liver failure secondary to infiltration of the liver by non-Hodgkin lymphoma.
Table 2.. Cases reported to date of acute liver failure secondary to infiltration of the liver by non-Hodgkin lymphoma. In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943174
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








