25 March 2024: Articles 
Lymphocytic Myocarditis with Increased Left Ventricular Thickness: A Rare Presentation Mimicking Cardiac Amyloidosis
Unusual clinical course, Mistake in diagnosis
Xueting Duan1ABCDEF, Liangzhen Qu1AEFG, Han Chen2ABEF*DOI: 10.12659/AJCR.942760
Am J Case Rep 2024; 25:e942760
Abstract
BACKGROUND: Lymphocytic myocarditis is an inflammatory condition of the heart that may present with a wide spectrum of symptoms and signs, ranging from asymptomatic to life-threatening cardiogenic shock and ventricular arrhythmia. Lymphocytic myocarditis usually presents as chamber dilation. However, increased left ventricular thickness is relatively rare. We present a case of lymphocytic myocarditis with increased left ventricular thickness which mimics the presentation of cardiac amyloidosis.
CASE REPORT: An 80-year-old Chinese man presented to the emergency room due to recurrent chest tightness. Wheezing and crackling were heard in both lungs, along with bilateral lower-extremity edema. He had elevated cardiac troponin T and N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels. Bedside echocardiogram showed left ventricular diastolic dysfunction and increased left ventricular thickness. Holter monitoring showed paroxysmal atrial fibrillation (AF) and atrial flutter. ⁹⁹ᵐTechnetium-pyrophosphate scintigraphy showed grade 1 myocardial uptake. Endomyocardial biopsy revealed lymphocytic myocarditis. The patient was put on steroids, managed with diuretics to alleviate the symptoms of congestion, and amiodarone for conversion of AF to sinus rhythm. He had no deterioration of cardiac function in the follow-ups, but there was still asymmetric interventricular septal hypertrophy.
CONCLUSIONS: Lymphocytic myocarditis may lead to increased left ventricular thickness in some rare cases. In the setting of unexplained increased left ventricular thickness, one should consider lymphocytic myocarditis as a differential diagnosis. In addition, endomyocardial biopsy should be performed as early as possible to confirm the diagnosis and identify the type of inflammation, which helps with treatment and prognosis.
Keywords: myocarditis, Hypertrophy, Left Ventricular, Biopsy, myocardial perfusion imaging
Introduction
Myocarditis is defined as an inflammatory infiltrate of the myocardium with myocyte degeneration and necrosis of nonischemic origin [1]. According to the type of infiltrated inflammatory cells, it could be classified as lymphocytic, eosinophilic with giant cells, or granulomatous, of which lymphocytic is the most prevalent [2].
The actual incidence of lymphocytic myocarditis is not well understood, as endomyocardial biopsy (EMB), the diagnostic criterion standard for myocarditis, is not widely applied in daily practice [3]. Lymphocytic myocarditis is mainly caused by viral infection, with a combination of direct virus-mediated or indirect immune-mediated myocardial injury, and it can also be an autoimmune process [4]. Of the viruses, parvovirus B19, adenovirus, and enterovirus have been identified as the most common pathogens [5].
Making the diagnosis of lymphocytic myocarditis is difficult, as clinical symptoms, cardiac markers, electrocardiogram (ECG), and echocardiography abnormalities are non-specific [5]. In the setting of clinically suspected myocarditis, cardiac magnetic resonance (CMR) imaging functions as a non-invasive tool to support the diagnosis of myocarditis based on the Lake Louise criteria. However, this approach will not yield information on infiltrated cell types [6]. EMB is essential for the definitive diagnosis of lymphocytic myocarditis, which is characterized by lymphocytes (CD3+ T lymphocytes) infiltrating the heart accompanied by signs of cardiomyocyte injury [2,7]. In addition, coronary angiography or computed tomography (CT) angiography also should be implemented to exclude acute coronary syndrome.
This report presents the case of an 80-year-old man with repeated chest tightness and increased left ventricular thickness, who was diagnosed with lymphocytic myocarditis until the implementation of endomyocardial biopsy.
Case Report
An 80-year-old man presented with recurrent chest tightness for about 2 months, with no symptoms of upper respiratory or digestive tract infection. He had a history of hypertension. He was vaccinated against COVID-19 in October 2021, March 2022, and August 2022. About 5 months previous to his presentation at our facility (February 2023), he experienced cough without fever, and, at the same time, his family members were infected with the SARS-CoV-2 virus. However, SARS- CoV-2 was not detected in the patient.
In May 2023, he visited a local doctor and was treated with piperacillin/tazobactam, doxofylline, and dexamethasone for about 1 week. However, his shortness of breath gradually progressed and he was transferred to a tertiary hospital. Laboratory findings on admission revealed elevated troponin T (0.037 ng/mL, normal value <0.014 ng/mL), creatine kinasemyocardial bound (CK-MB) (36 U/L, normal value <24 U/L), and N-terminal pro-B-type natriuretic peptide (NT-proBNP) (3958 pg/mL, normal value <125 pg/mL) levels, with normal complete blood cell count and C-reactive protein (CRP) levels. The ECG reported atrial fibrillation (AF), mild ST segment elevation in leads V3 and V4, and T-wave change in leads II, III, aVF, V5, and V6 (Figure 1). The echocardiography showed biatrial enlargement with mild mitral regurgitation, mild aortic regurgitation, and mild to moderate tricuspid regurgitation. Additionally, trivial pericardial effusion was observed. A chest CT revealed chronic bronchitis and emphysema in both lungs.
After admission, the patient progressed to worsened shortness of breath, with loud wheezing sounds in both lungs. Bronchial asthma was suspected, and we had initially treated the patient with methylprednisolone and diuretics. On the third day of hospitalization, bedside ultrasound showed moderate right pleural effusion. Thus, the patient underwent chest drainage. Then the symptoms gradually improved and he was discharged with methylprednisolone tablets.
In July 2023, he developed chest tightness again and was sent to our hospital. On admission, the patient’s body temperature was 36.9°C, pulse was 81 beats per minute, respiratory rate was 18 breaths per minute and blood pressure was 96/58 mmHg. Respiratory sounds were coarse and wheezing sounds could be heard in both lungs. He had no edema and no skin lesions.
His white blood cell count, neutrophil count, and lymphocyte count were normal, but CRP (68 mg/L, normal value <10 mg/L) and interleukin-6 (25.4 pg/mL, normal value <7 pg/mL) were elevated. Cardiac markers were slightly elevated, with an NT-proBNP level of 1983 ng/L and a troponin T level of 0.082 ng/ mL, but with normal creatine kinase (CK) and CK-MB levels.
The results of blood free light chains, immunoglobulin classes, and serum immunofixation electrophoresis were negative except for elevated free Kappa light chain (46.19 mg/L), a reduced light chain κ/λ ratio (1.28), and elevated C3 (1.42 g/L). Sputum culture showed
ECG revealed sinus or ectopic atrial rhythm, atrial premature beat, left ventricular high voltage, prolonged QT interval, and possible lateral wall infarction. The echocardiography showed asymmetrical left ventricular hypertrophy, and the maximum interventricular septal thickness was 1.63 cm, raising concern for hypertrophic cardiomyopathy (Figure 2A). In addition, the mitral valve and aortic valve were also thickened. Left ventricular (LV) ejection fraction was 61.9%, with decreased left ventricular diastolic function. 99mTechnetium-pyrophosphate (99mTc-PYP) myocardial scintigraphy showed grade 1 myocardial uptake.
Endomyocardial biopsy was performed on suspicion of myocar-dial amyloidosis; however, the pathology revealed lymphocytic myocarditis, with diffuse small and focal large lymphomonocyte infiltration (>14/mm2), cardiomyocyte degeneration/necrosis, and focal fibrosis (Figure 3A, 3B). Immunohistochemistry showed interstitial expression of Kappa foci and no Lambda or amyloid A protein (Figure 3C, 3D).
The patient was then treated with piperacillin/tazobactam (4.5 g/8 h), tolvaptan (15 mg/d), torsemide (5 mg/d), amiodarone (200 mg/d), rivaroxaban (10 mg/d), and ivabradine (5 mg/d). He was observed at hospital for 12 days and discharged with oral medications.
At the patient’s 2-week follow-up visit, he reported no symptoms and had a normal NT-proBNP level. The echocardiography showed normal cardiac size and function. However, the asymmetric interventricular septal hypertrophy remained, and his maximum interventricular septal thickness was 1.71 cm (Figure 2B).
Discussion
To the best of our knowledge, we present the first case describing increased left ventricular thickness in lymphocytic myocarditis, emphasizing the importance of early implementation of endomyocardial biopsy.
Arriving at a diagnosis of lymphocytic myocarditis is challenging. Clinically, lymphocytic myocarditis may manifest as subclinical disease, arrhythmia, heart failure, and even sudden cardiac death. Symptoms are nonspecific, including dyspnea, chest pain, palpitation, and arrhythmia. Laboratory biomarkers such as CRP, troponin, CK, and B-type natriuretic peptide (BNP) are also non-specific. Although cardiac troponin levels are more sensitive in patients with clinically suspected myocarditis than CK levels, normal levels of either of these biomarkers do not exclude myocarditis [8]. ECG findings, including atrioventricular block, bundle branch block, or ST/T-wave change, are neither specific nor sensitive. Our patient presented with symptoms of chest tightness and elevated troponin level.
Common findings in echocardiograms include impaired left ventricular systolic function and increased left ventricular diameter. Inflammation may cause extensive scarring that triggers LV remodeling, eventually leading to dilated cardiomyopathy [9] or a predominant hypokinetic nondilated phenotype of cardiomyopathy. In contrast, our patient presented with increased LV thickness, which is typically a manifestation of fulminant myocarditis [10]. In addition, several cases of non-fulminant myocarditis mimicking hypertrophic cardiomyopathy with transient LV wall thickening, caused by influenza virus or adenovirus, have also been reported [11,12], but the type of myocarditis is unknown. We present a histopathologically confirmed case of lymphocytic myocarditis that presented with LV wall thickening that was still evident at a 2-week follow-up. However, this follow-up time is relatively short, and LV wall thickening may resolve during further cardiology follow-up. Moreover, we did not perform a viral infection screen or autoantibody serum testing to identify the cause of the lymphocytic myocarditis. Therefore, we could not determine the association between lymphocytic myocarditis and COVID-19 vaccination or SARS-CoV-2 infection.
CMR is the best noninvasive test recommended by the guidelines [3].The infiltration of inflammatory cells into the myocardium leads to myocardial edema, and subsequently hyperemia, necrosis, and fibrosis, which are well visualized by CMR. The Lake Louis Criteria of CMR has a sensitivity of 67% and specificity of 91% in making the diagnosis of myocarditis [6].
As a functional imaging tool, 18F-fluoro-deoxy-glucose (FDG) positron emission tomography/CT (PET/CT), has a potential role in the assessment of myocarditis by providing metabolic information on inflammation as increased myocardial FDG uptake [13]. Case-based observational studies have suggested complementary and incremental values of FDG PET/CT/ CMR in the assessment of myocarditis, compared with PET/ CT or CMR alone [14].
According to the results of 99mTc-PYP myocardial imaging and the echocardiogram, this patient was once suspected to have cardiac amyloidosis. As is well-known, cardiac amyloidosis is characterized by the extracellular deposition of misfolded proteins in the heart. The most common misfolded proteins are monoclonal immunoglobulin light chains or transthyretin (ATTR). ATTR can be diagnosed based solely on non-invasive diagnostic criteria, with typical echocardiographic/CMR findings, grade 2 or 3 myocardial uptake in diphosphonate scintigraphy and negative monoclonal proteins [15].
EMB is the criterion standard for the diagnosis of both myocarditis and cardiac amyloidosis [16], which are respectively characterized by inflammatory cell infiltration with myocyte degeneration and necrosis [3], and the pathognomonic histological property of green birefringence when viewed under cross-polarized light after staining with Congo red [15]. Except for confirming the diagnosis of myocarditis, EMB also identifies the underlying etiology and the type of inflammation, which imply different treatments and prognosis. However, EMB is an invasive test with potential perceived risks and is performed infrequently in real practice. Moreover, the sensitivity of EMB for lymphocytic myocarditis is relatively low [17].
Conclusions
We hereby present a case of lymphocytic myocarditis with increased LV thickness, which was at first suspected to be myocardial amyloidosis. The phenomenon is rare. However, physicians should realize this possible manifestation, and early EMB should be performed to avoid potential misdiagnosis. LV hypertrophy may be reversible, so it is necessary to check the echocardiogram during follow-ups.
Figures
Tables
. Timeline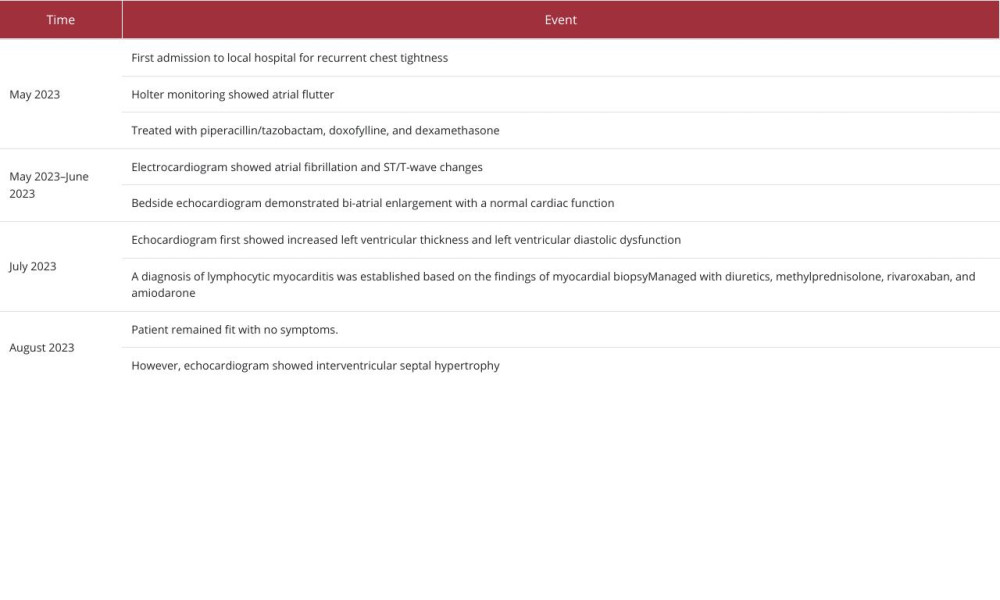
References
1.. Aretz HT, Billingham ME, Edwards WD, Myocarditis. A histopathologic definition and classification: Am J Cardiovasc Pathol, 1987; 1(1); 3-14
2.. Ammirati E, Frigerio M, Adler ED, Management of acute myocarditis and chronic inflammatory cardiomyopathy: An expert consensus document: Circ Heart Fail, 2020; 13(11); e007405
3.. Caforio AL, Pankuweit S, Arbustini E, Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases: Eur Heart J, 2013; 34(33); 2636-48 , 2648a–2648d
4.. Indraratna P, Sivasubramaniam V, Davidson T, Eggleton S, A case report of isolated right ventricular lymphocytic myocarditis: Eur Heart J Case Rep, 2020; 4(4); 1-5
5.. Lam L, Sathirareuangchai S, Oyama J, Lymphocytic myocarditis and cardiogenic shock in Hawai’i: A case series: Hawaii J Health Soc Welf, 2019; 78(7); 223-29
6.. Friedrich MG, Sechtem U, Schulz-Menger J, Cardiovascular magnetic resonance in myocarditis: A JACC White Paper: J Am Coll Cardiol, 2009; 53(17); 1475-87
7.. Nagai T, Inomata T, Kohno T, JCS 2023 Guideline on the diagnosis and treatment of myocarditis: Circ J, 2023; 87(5); 674-54
8.. Lauer B, Niederau C, Kühl U, Cardiac troponin T in patients with clinically suspected myocarditis: J Am Coll Cardiol, 1997; 30(5); 1354-59
9.. Towbin JA, Lowe AM, Colan SD, Incidence, causes, and outcomes of dilated cardiomyopathy in children: JAMA, 2006; 296(15); 1867-76
10.. Kociol RD, Cooper LT, Fang JC, Recognition and initial management of fulminant myocarditis: A Scientific Statement from the American Heart Association: Circulation, 2020; 141(6); e69-e92
11.. Aydin A, Ali F, Khariton M, Spencer R, A teenager with adenoviral myocarditis mimicking hypertrophic cardiomyopathy: Cardiol Young, 2023; 33(10); 2110-12
12.. Giafaglione JR, Morrison AK, Nandi D, A case report of myocarditis masquerading as hypertrophic cardiomyopathy: Ann Pediatr Cardiol, 2020; 13(4); 340-42
13.. Chen W, Jeudy J, Assessment of myocarditis: Cardiac MR, PET/CT, or PET/ MR: Curr Cardiol Rep, 2019; 21(8); 76
14.. von Olshausen G, Hyafil F, Langwieser N, Detection of acute inflammatory myocarditis in Epstein Barr virus infection using hybrid 18F-fluorodeoxyglucose-positron emission tomography/magnetic resonance imaging: Circulation, 2014; 130(11); 925-26
15.. Garcia-Pavia P, Rapezzi C, Adler Y, Diagnosis and treatment of cardiac amyloidosis: A position statement of the ESC Working Group on Myocardial and Pericardial Diseases: Eur Heart J, 2021; 42(16); 1554-68
16.. Cooper LT, Baughman KL, Feldman AM, The role of endomyocardial biopsy in the management of cardiovascular disease: A Scientific Statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology Endorsed by the Heart Failure Society of America and the Heart Failure Association of the European Society of Cardiology: Eur Heart J, 2007; 28(24); 3076-93
17.. Chow LH, Radio SJ, Sears TD, McManus BM, Insensitivity of right ventricular endomyocardial biopsy in the diagnosis of myocarditis: J Am Coll Cardiol, 1989; 14(4); 915-20
Figures
Tables
In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








